 |
 |
| Korean J Ophthalmol > Volume 37(1); 2023 > Article |
|
Abstract
Purpose
To investigate whether postoperative filtering bleb size affects the surgical outcome after trabeculectomy.
Methods
In this study, we retrospectively reviewed 145 medically uncontrolled glaucoma patients with intraocular pressure (IOP) values >21 mmHg before surgery and data from ≥2 years of follow-up. Postoperative IOP, filtering bleb size including extent and height, and other clinical factors were measured after trabeculectomy. We divided bleb extent into quadrants and bleb height by 0.5 intervals of corneal thickness. The main outcome measure was surgical success. We confirmed complete success when the IOP was ≤21 mmHg and decreased by >20% from baseline without medication or additional procedures. Qualified success used the same criteria but allowed for medication or additional procedures. Cases with reoperation or two consecutive IOP measurements <6 mmHg were considered failures.
Results
A total of 145 eyes of 145 patients was included. The average observation period was 30.8 ± 10.9 months. During multivariate Cox regression analysis, a larger extent of filtering bleb revealed significantly low hazard ratios in both complete and surgical success (0.509 and 0.494, respectively); however, there was no significant relationship between bleb height and surgical outcome.
Trabeculectomy is a well-known surgical procedure in glaucoma patients with failed control of intraocular pressure (IOP) [1-3]. Nevertheless, some patients suffer surgical failure, and their IOP increases again, requiring additional treatment such as needling or reoperation [3]. Several factors, including type of glaucoma [3], race [4], diabetes [5], previous ocular surgery [6,7], and long-term use of glaucoma medication [8-10], were reported to affect the surgical outcome of trabeculectomy. In addition, the characteristics of the filtering bleb, such as bleb size, vascularity, and reflectivity, have been reported to be associated with surgical prognosis [11-13].
The leading cause of failure appears to be a progressive cicatricial course of the scleral and subconjunctival tissue around the filtering bleb. Scar formation in the surgical area can reduce bleb height or extent and decrease the outflow volume of aqueous humor, leading to surgical failure. Therefore, surgical success seems to be dependent on proper maintenance of the filtering bleb [14-19]. Several studies have demonstrated the relationship between filtering bleb morphology and surgical prognosis. However, these previous studies mostly observed patients for a relatively short period <12 months or only investigated the characteristics of filtering blebs [20-22]. Therefore, it is necessary to examine whether filtering blebs affect the surgical outcome over a longer period of time. Under the hypothesis that there will be a correlation between maintenance of filtering bleb size and postoperative IOP, this study was performed to determine the association between bleb extent or height and surgical outcome of trabeculectomy. In addition, we also investigated other factors such as previous glaucoma surgery history, type of glaucoma, duration of mitomycin C (MMC) application, and number of antiglaucoma medications that could affect the surgical outcomes during a long-term follow-up period ≥2 years postoperatively.
This study was approved by the Institutional Review Board of Samsung Medical Center (No. 2021-08-070) and was performed in accordance with the Declaration of Helsinki. Informed consent was exempted due to retrospective study design and use of anonymized clinical data.
In this study, we retrospectively analyzed the medical records of 145 patients who had undergone trabeculectomy between January 2009 and July 2013 performed by a single surgeon (BHA) with ≥2 years of follow-up data. Demographic characteristics of age, sex, central corneal thickness (CCT), refractive error, glaucoma diagnosis, IOP, number of IOP-lowering medications, and use of additional treatments were collected by medical records review. Goldmann applanation tonometry was performed to measure IOP.
Patients with IOP >21 mmHg and medically uncontrolled glaucoma were enrolled in this study. We analyzed the medical charts of patients aged >18 years with primary open-angle glaucoma (POAG); chronic angle-closure glaucoma (CACG); and secondary glaucoma including neovascular glaucoma, uveitic glaucoma, steroid-induced glaucoma, pigmentary glaucoma, and pseudoexfoliation glaucoma. Meanwhile, we excluded patients who had undergone any other ocular surgeries except phacoemulsification and previous filtering operations. When both eyes of the patient met the inclusion criteria, data from the earlier operated eye were used.
All surgeries were performed under general or local anesthesia using a fornix-based conjunctival incision by a single surgeon (BHA) who had no preference for either trabeculetomy or phacotrabeculetomy.
Tractional suturing to the limbus was performed with 7-0 black silk. Local anesthesia was conducted by subconjunctival injection of 2% lidocaine. Tenon’s layer (or capsule) was dissected and extended, and a partial thickness of lamellar scleral flap formation was adopted. Exposed scleral tissues were treated with 0.02% or 0.04% MMC or sponges soaked in MMC for 1 to 4 minutes and gently washed with balanced salt solution. An anterior chamber paracentesis was created on the temporal side, and sclerotomy with peripheral iridectomy was conducted. Scleral flap reapproximation was performed with interrupted 10-0 nylon sutures, and the conjunctival flap was closed using 10-0 nylon.
A balanced salt solution was injected into the anterior chamber, and the surgeon assessed the leakage rate of the filtering bleb. When the IOP was adequate and the outflow of the aqueous humor was appropriate, the operation was followed by application of ofloxacin ointment and placement of an eye patch.
After the surgery, a topical moxifloxacin hydrochloride 0.5% solution (Vigamox, Alcon Laboratories) was instilled for about 1 month, and a topical steroid prednisolone acetate 1% eyedrop (Pred Forte, Allergan) was prescribed to be used four times a day for about 3 months postoperatively.
With reference to the virgin conjunctiva and sclera before surgery, bleb analysis consisted of the two parameters of bleb height and extent. Both were assessed during a slit-lamp examination performed by the same glaucoma specialist (BHA) who performed each surgery. The parameters were evaluated at 1 and 2 weeks; 1, 3, and 6 months; 1 year; and then every year thereafter. However, we included only data collected at 1, 3, and 6 months; 1 year; and every year thereafter in our analysis.
First, for bleb height, the thickness of the cystic space between the bleb wall was graded from 0CCT to 4CCT in 0.5 intervals based on the CCT by the surgeon (BHA). For example, when the thickness of the filtering bleb space was twice that of the CCT, it was denoted as 2CCT; when the bleb was flat, we described it as 0CCT. Second, for bleb extent, the morphology was drawn on the medical chart by the surgeon and divided into quadrants (Q) according to the area occupied. The area of the bleb extent was categorized from 0Q to 4Q depending on the corresponding quadrant; for example, if the extent of the bleb figure occupied only a single quadrant, it was described as 1Q. Similar to the bleb height, when the bleb was flat, it was described as 0Q (Fig. 1A-1F).
The primary outcome measure was surgical success, and the main criterion for surgical success was IOP. Complete success was defined as IOP ≤21 mmHg and a >20% reduction in preoperative IOP without any additional treatment. If additional treatment, including in-clinic intervention or glaucoma medication, was required to achieve the same IOP as needed to define complete success, then the patient was considered to have achieved qualified success. Surgical failure was defined when the IOP was >21 or <6 mmHg at two consecutive measurements or when additional filtering surgery was required.
Cox regression analysis was conducted to show the correlation between filtering bleb size and surgical success of trabeculectomy. Hazard ratio (HR) was described using mean and 95% confidence interval in univariate and multivariate analyses. Kaplan-Meier survival curves were used to assess the success of trabeculectomy according to complete and qualified success criteria. All statistical tests were performed using the R ver. 3.6.3 (R Foundation for Statistical Computing), and p-values of <0.05 were considered to be statistically significant. In this study, we used the readily available R function cox.zph, which is available in the R core package survival, to test the proportional hazards assumption [23].
The baseline characteristics of the enrolled patients are shown in Table 1. A total of 145 eyes of 145 patients with medically uncontrolled glaucoma were analyzed. Ninety-five male patients (65.5%) and 50 female patients (34.5%) aged 20 to 87 years underwent trabeculectomy. The preoperative mean values of age, CCT, refractive error (spherical equivalent), and maximum IOP were 59.5 ± 14.2 years, 526.8 ± 34.6 μm, −1.8 ± 3.6 diopters, and 31.9 ± 9.7 mmHg, respectively. The mean number of medications used before surgery was 2.7 ± 0.9. There were 27 patients (18.6%) with a history of previous glaucoma surgery.
Among the 145 eyes included in the study, 115 patients (79.3%) underwent only trabeculectomy and 35 patients (20.7%) underwent trabeculectomy with phacoemulsification. The types of glaucoma diagnosed comprised POAG, CACG, and secondary glaucoma; of these, POAG was the most common diagnosis, with 101 cases (69.7%), followed by CACG with 27 cases (18.6%) and secondary glaucoma with 17 cases (11.7%). Success rates of total patients were 20.7% in complete succuss and 80.7% in qualified success at 24 months postoperatively (Table 2).
The univariate and multivariate logistic regression analyses of complete success are shown in Table 3 and Supplementary Tables 1-6. We described the univariate analysis (model 1), the results of stepwise multivariate analysis that were adjusted only for age and sex (model 2), and the results of the adjustment for variables that were significant in the univariate analysis (model 3) in Table 3. We analyzed associations between surgical success and variables of sex, CCT, refractive error, history of glaucoma surgery, type of glaucoma, MMC soaking time of the tissue, preoperative IOP, and bleb parameters (height or extent) 1 month after trabeculectomy. To avoid statistical confounding, bleb height and extent were analyzed separately in a multivariate analysis of complete and qualified success. Table 3 and the aforementioned Supplementary Tables 1-6 show the results of the multivariate Cox proportional hazard test by excluding extent or height of the filtering bleb. The bleb extent was significantly correlated in both univariate and multivariate analyses of qualified and complete success, and height had no significant result in any outcome at 1 month and 3 months postoperatively. However, only the bleb height was significantly associated with surgical success at postoperative 6 months. Subset analyses were performed according to the lens status (phakia or pseudophakia) and whether the trabeculectomy was accompanied by phacoemulsification. There was a significant association between complete success and bleb extent at 1 and 3 months after surgery in all subanalyses except for patients with pseudophakia (Supplementary Tables 1, 3, 4). In patients of pseudophakia, the larger bleb extent had lower HR only for complete success at 3 months postoperatively (HR, 0.446) (Supplementary Table 2).
Stepwise multivariate logistic regression was performed. Considering complete success, CACG patients tended to have better surgical outcomes compared to POAG patients (HR, 0.398). The extent of filtering bleb also had a negative relationship (complete sucess HR, 0.530; qualified sucess HR, 0.545), but previous glaucoma surgery increased the risk of surgical failure (complete sucess HR, 1.784; qualified sucess HR, 2.791) in both complete and qualified success. Male patients had a significantly low risk compared to female patients (HR, 0.461) in the category of qualified success (Supplementary Tables 5, 6).
In addition, we divided patients into two groups by bleb size, i.e., ≥2Q or ≥2CCT and <2Q or <2CCT. Considering bleb height, there was no significant difference in the HR of surgical failure between the ≥2CCT and <2CCT groups. However, for extent, the ≥2Q group had a significantly lower risk than the <2Q group in the category of qualified success after adjusting for other variables and in complete success with or without adjusting for other factors (Tables 4, 5).
We calculated the results through Kaplan-Meier survival analysis (Fig. 2A, 2B). Significant difference was shown in adjusted HR for complete success and qualified success (p < 0.001 and p = 0.02, respectively), with a reduced risk of surgical failure for extent of the ≥2Q group (Fig. 2A, 2B, 3A, 3B).
In this study, we investigated the relationships between bleb parameters and surgical outcome after trabeculectomy over a long-term postoperative period averaging 30.8 ± 10.9 months. A larger extent size of the filtering bleb at 1 month after trabeculectomy was significantly associated with a good surgical prognosis. The present result is consistent with previous study findings. Kawana et al. [20] revealed good surgical outcomes in glaucoma eyes with large surgical blebs using anterior segment optical coherence tomography (OCT). Hamanaka et al. [21] evaluated bleb morphology with the Indiana Bleb Appearance Grading Scale (IBAGS) and OCT after limbal-based trabeculectomy and found that a wide extent of blebs ensured good IOP control. With this study, we add stronger evidence to the literature to confirm that early filtering bleb morphology, especially at 1 month after surgery, is important to predict the long-term surgical outcome of trabeculectomy.
In the present study, the bleb extent and height were evaluated only through slit-lamp examination like previous studies [24-26]. Measurement of bleb parameters through a slit-lamp is convenient and has the advantage of being cost-effective and time-effective as the patient does not require additional examinations. However, the internal structure of the bleb also can be observed with ultrasound biomicroscopy and OCT imaging [22,27,28]. Long-term follow-up studies using these devices evaluating filtering blebs are needed in the future.
The present study indicated that the extent of filtering bleb is significantly related to surgical outcome of trabeculectomy, but the explanations for this result remain unclear. After the aqueous humor passes through the internal ostium from the anterior chamber, it enters the transconjunctival space (transconjunctival filtration), lymphatic system, or episcleral venous plexus [29]. Therefore, maintenance of the bleb after filtration surgery is directly related to outflow of aqueous humor, and it is important to maintain filtering bleb morphology without leading to a cicatricial process. Under this point of view, the boundary of the extent seems to reflect the practical area of the functioning bleb and might be associated with surgical outcome [11,12].
The height of the filtering bleb was not significantly related to surgical prognosis in the present study. Singh et al. [22] reported results consistent with ours after analyzing the structure of successful blebs by comparing color photographs of blebs captured with anterior segment OCT, and they found that bleb height did not have an association with bleb cavities. High blebs could include both small and large internal cavities, which are heterogeneous in terms of wall thickness. On the other hand, Kawana et al. [20] defined total bleb height as the maximum distance between the internal surface of the intrableb fluid-filled cavity and the bleb surface using OCT and determined the association with IOP through Spearman correlation. In their study, IOP showed a significant negative correlation with total bleb height.
In the present study, factors other than bleb extent were related with a good surgical outcome. CACG as opposed to POAG, no history of previous glaucoma surgery, and male sex were factors associated with good surgical outcome in univariate and multivariate analyses. Some of these results are consistent with previous study findings. Law et al. [6] and Cankaya and Elgin [7] reported better surgical outcomes of initial trabeculectomy compared to repeat trabeculectomy. This might be because intraocular surgery disrupts the blood-aqueous barrier, which in turn alters components such as growth factors of aqueous humor, resulting in changes in the wound-healing process. As a result, the conjunctiva of patients with a history of such surgeries contains larger numbers of fibroblasts and inflammatory cells [30]. In a previous study, CACG patients had lower risk than POAG patients in terms of both complete (HR, 0.6; 95% confidence interval, 0.20-2.70) and qualified success (HR, 0.3; 95% confidence interval, 0.02-7.70), but the differences were not statistically significant
It is important to predict surgical outcome with bleb morphology in the early postoperative period. After trabeculectomy, early interventions, such as needling and laser suture lysis, might be required due to wound-healing and the cicatricial process of the filtering bleb, which could impede outflow of aqueous humor. Since it is difficult to predict the long-term surgical prognosis, it is necessary to evaluate clinical factors that might be associated with the surgical outcome. Therefore, these findings might contribute to determining more appropriate interventions in the early postoperative period and could predict successful trabeculectomy over a long-term follow-up period.
This study has several limitations. First, it was limited by its retrospective study design. Second, there is a possibility that the internal structure of the bleb was not properly evaluated because measurements of bleb size were performed during slit-lamp examinations. The extent of the filtering bleb was categorized as 0Q to 4Q, according to the quadrant of surgeons’ medical chart drawing, and the height was denoted based on the CCT range from 0CCT to 4CCT. This decision was based arbitrarily by modifications of IBAGS and Moorfields Bleb Grading System (MBGS). However, the grading was performed by a single experienced surgeon with a consistent method to minimize bias induced by different measurers. Additionally, as only the height and extent of the bleb morphology were measured in this study, and a long-term study including other factors, such as vascularity, bleb wall thickness, and other internal structures of the filtering bleb, is necessary.
In conclusion, it seems that there is an association between various factors including filtering bleb extent and surgical outcomes over long-term follow-up.
Acknowledgements
The authors thank Da-Hyeun Lee, the audiovisual engineer at Samsung Medical Information & Medical Services, Samsung Medical Center, for designing Fig. 1 in this study.
Supplementary Materials
Supplementary materials are available from https://doi.org/10.334/kjo.2022.0082.
Supplementary Table 1.
Univariate and multivariate Cox regression analyses of success in patients with phakia
Supplementary Table 2.
Univariate and multivariate Cox regression analyses of success in patients with pseudophakia (n = 36)
Supplementary Table 3.
Univariate and multivariate Cox regression analyses of success in patients with only trabeculectomy (n = 115)
Supplementary Table 4.
Univariate and multivariate Cox regression analyses of success in patients of trabeculectomy with phacoemulsification (n = 30)
Supplementary Table 5.
Univariate and stepwise multivariate Cox regression analyses of complete success after surgery (n = 145)
Supplementary Table 6.
Univariate and stepwise multivariate Cox regression analyses of qualified success after surgery (n = 145)
References
2. Watson PG, Barnett F. Effectiveness of trabeculectomy in glaucoma. Am J Ophthalmol 1975;79:831-45.


3. Landers J, Martin K, Sarkies N, et al. A twenty-year follow-up study of trabeculectomy: risk factors and outcomes. Ophthalmology 2012;119:694-702.


4. Broadway D, Grierson I, Hitchings R. Racial differences in the results of glaucoma filtration surgery: are racial differences in the conjunctival cell profile important? Br J Ophthalmol 1994;78:466-75.



5. Edmunds B, Bunce CV, Thompson JR, et al. Factors associated with success in first-time trabeculectomy for patients at low risk of failure with chronic open-angle glaucoma. Ophthalmology 2004;111:97-103.


6. Law SK, Shih K, Tran DH, et al. Long-term outcomes of repeat vs initial trabeculectomy in open-angle glaucoma. Am J Ophthalmol 2009;148:685-95e1.


7. Cankaya AB, Elgin U. Comparison of the outcome of repeat trabeculectomy with adjunctive mitomycin C and initial trabeculectomy. Korean J Ophthalmol 2011;25:401-8.



8. Broadway DC, Grierson I, O’Brien C, Hitchings RA. Adverse effects of topical antiglaucoma medication: II. The outcome of filtration surgery. Arch Ophthalmol 1994;112:1446-54.


9. Miki T, Naito T, Fujiwara M, et al. Effects of pre-surgical administration of prostaglandin analogs on the outcome of trabeculectomy. PLoS One 2017;12:e0181550..


10. Hoang TK, Kim YK, Jeoung JW, Park KH. Relationship between age and surgical success after trabeculectomy with adjunctive mitomycin C. Eye (Lond) 2018;32:1321-8.




11. Yin X, Cai Q, Song R, et al. Relationship between filtering bleb vascularization and surgical outcomes after trabeculectomy: an optical coherence tomography angiography study. Graefes Arch Clin Exp Ophthalmol 2018;256:2399-405.



12. Kokubun T, Tsuda S, Kunikata H, et al. Anterior-segment optical coherence tomography for predicting postoperative outcomes after trabeculectomy. Curr Eye Res 2018;43:762-70.


13. Tsutsumi-Kuroda U, Kojima S, Fukushima A, et al. Early bleb parameters as long-term prognostic factors for surgical success: a retrospective observational study using three-dimensional anterior-segment optical coherence tomography. BMC Ophthalmol 2019;19:155.




14. Addicks EM, Quigley HA, Green WR, Robin AL. Histologic characteristics of filtering blebs in glaucomatous eyes. Arch Ophthalmol 1983;101:795-8.


15. Costa VP, Spaeth GL, Eiferman RA, Orengo-Nania S. Wound healing modulation in glaucoma filtration surgery. Ophthalmic Surg 1993;24:152-70.


16. Maumenee AE. External filtering operations for glaucoma: the mechanism of function and failure. Trans Am Ophthalmol Soc 1960;58:319-28.


17. Skuta GL, Parrish RK. Wound healing in glaucoma filtering surgery. Surv Ophthalmol 1987;32:149-70.


18. Broadway DC, Chang LP. Trabeculectomy, risk factors for failure and the preoperative state of the conjunctiva. J Glaucoma 2001;10:237-49.


19. Wong TT, Mead AL, Khaw PT. Prolonged antiscarring effects of ilomastat and MMC after experimental glaucoma filtration surgery. Invest Ophthalmol Vis Sci 2005;46:2018-22.


20. Kawana K, Kiuchi T, Yasuno Y, Oshika T. Evaluation of trabeculectomy blebs using 3-dimensional cornea and anterior segment optical coherence tomography. Ophthalmology 2009;116:848-55.


21. Hamanaka T, Omata T, Sekimoto S, et al. Bleb analysis by using anterior segment optical coherence tomography in two different methods of trabeculectomy. Invest Ophthalmol Vis Sci 2013;54:6536-41.


22. Singh M, Chew PT, Friedman DS, et al. Imaging of trabeculectomy blebs using anterior segment optical coherence tomography. Ophthalmology 2007;114:47-53.


23. Grambsch PM, Therneau TM. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 1994;81:515-26.

24. Kronfeld FC. The chemical demonstration of transconjunctival passage of aqueous after antiglaucomatous operations. Am J Ophthalmol 1952;35:38-45.


25. Cantor LB, Mantravadi A, WuDunn D, et al. Morphologic classification of filtering blebs after glaucoma filtration surgery: the Indiana Bleb Appearance Grading Scale. J Glaucoma 2003;12:266-71.


26. Wells AP, Crowston JG, Marks J, et al. A pilot study of a system for grading of drainage blebs after glaucoma surgery. J Glaucoma 2004;13:454-60.


27. Yamamoto T, Sakuma T, Kitazawa Y. An ultrasound biomicroscopic study of filtering blebs after mitomycin C trabeculectomy. Ophthalmology 1995;102:1770-6.


28. Savini G, Zanini M, Barboni P. Filtering blebs imaging by optical coherence tomography. Clin Exp Ophthalmol 2005;33:483-9.


Fig. 1
A representative case of the bleb after trabeculectomy in a patient with uveitic glaucoma. (A) A medical chart’s drawing of bleb morphology by the surgeon, (B) slit-lamp photographs of the bleb under narrow beam, and (C) diffuse illumination at 1 month postoperatively. (D) A medical chart’s drawing and (E,F) slit-lamp photographs of the bleb at 2 years postoperatively. We evaluated the patient’s bleb as 3 central corneal thickness (3CCT) and 1 quadrant (1Q) at postoperative 1 month, and 2CCT and 2Q at postoperative 2 years. The height of filtering bleb (FB) was three times of CCT and the extent occupied only a single Q at 1 month after surgery. Those of postoperative 2 years corresponded to twice of CCT and two Qs of the area.

Fig. 2
Kaplan-Meier survival analysis of complete success rates of groups according to bleb size, i.e., eyes with bleb size <2 (red line) and eyes with bleb size ≥2 (blue line). (A) The height was evaluated at 0.5 intervals based on the central corneal thickness (CCT) ranging from 0CCT to 4CCT. (B) The bleb extent was divided into quadrants (Qs) from 0Q to 4Q.
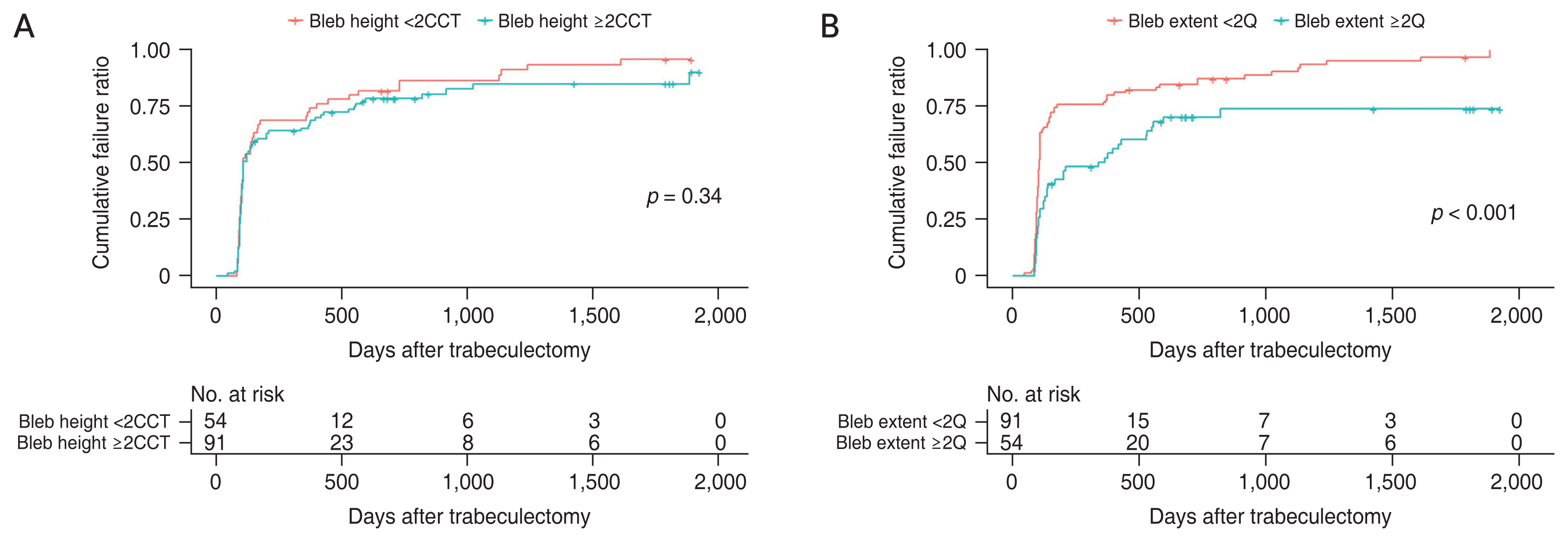
Fig. 3
Kaplan-Meier survival analysis of qualified success rates of groups according to bleb size, i.e., eyes with bleb size <2 (red line) and eyes with bleb size ≥2 (blue line). (A) The height was evaluated at 0.5 intervals based on the central corneal thickness (CCT) ranging from 0CCT to 4CCT. (B) The bleb extent was divided into quadrants (Qs) from 0Q to 4Q.
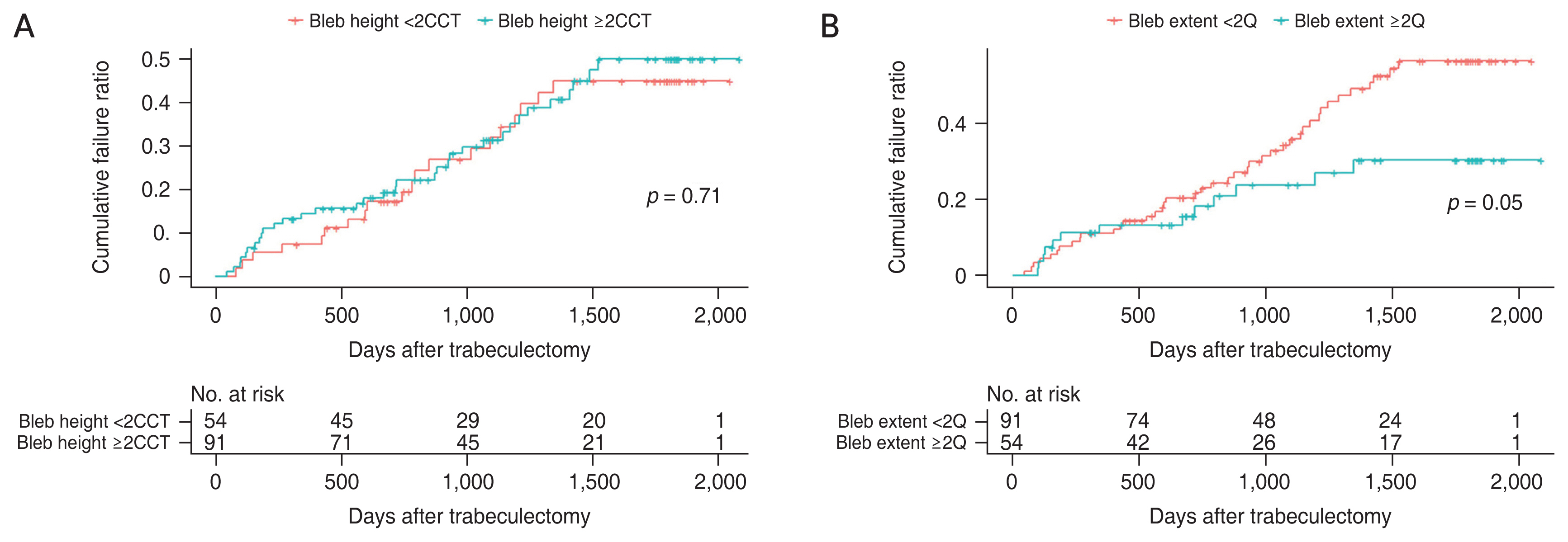
Table 1
Baseline characteristics (n = 145)
Table 2
Overall complete success rate and overall qualified success rate
| Postoperative | Complete success (%) | Qualified success (%) |
|---|---|---|
| 1 mon | 100 | 100 |
| 3 mon | 87.6 | 97.9 |
| 6 mon | 36.6 | 92.4 |
| 12 mon | 32.4 | 88.3 |
| 24 mon | 20.7 | 80.7 |
Table 3
Univariate and multivariate Cox regression analyses of success
| Variable | Complete success (20%) | Qualified success (20%) | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| HR | 95% CI | p-value | HR | 95% CI | p-value | |
| Bleb height at 1 mon | ||||||
| Model 1 | 0.870 | 0.674-1.123 | 0.284 | 0.905 | 0.606-1.351 | 0.626 |
| Model 2 | 0.819 | 0.623-1.076 | 0.152 | 0.945 | 0.613-1.458 | 0.798 |
| Model 3 | 0.844 | 0.643-1.108 | 0.221 | 0.969 | 0.615-1.527 | 0.893 |
| Bleb extent at 1 mon | ||||||
| Model 1 | 0.543 | 0.393-0.751 | <0.001* | 0.575 | 0.331-0.997 | 0.049* |
| Model 2 | 0.545 | 0.392-0.757 | <0.001* | 0.503 | 0.334-1.018 | 0.058 |
| Model 3 | 0.530 | 0.384-0.730 | <0.001* | 0.545 | 0.311-0.955 | 0.034* |
| Bleb height at 3 mon | ||||||
| Model 1 | 0.947 | 0.714-1.257 | 0.707 | 0.593 | 0.375-0.936 | 0.025 |
| Model 2 | 0.866 | 0.635-1.179 | 0.360 | 0.484 | 0.288-0.813 | 0.006 |
| Model 3 | 0.847 | 0.608-1.179 | 0.326 | 0.476 | 0.273-0.830 | 0.009 |
| Bleb extent at 3 mon | ||||||
| Model 1 | 0.546 | 0.389-0.765 | <0.001* | 0.330 | 0.192-0.566 | <0.001* |
| Model 2 | 0.560 | 0.396-0.791 | 0.001* | 0.291 | 0.164-0.514 | <0.001* |
| Model 3 | 0.542 | 0.385-0.765 | <0.001* | 0.265 | 0.150-0.469 | <0.001* |
| Bleb height at 6 mon | ||||||
| Model 1 | 0.820 | 0.632-1.063 | 0.134 | 0.588 | 0.405-0.855 | 0.005* |
| Model 2 | 0.721 | 0.540-0.963 | 0.027* | 0.511 | 0.339-0.770 | 0.001* |
| Model 3 | 0.697 | 0.517-0.939 | 0.018* | 0.544 | 0.342-0.865 | 0.010* |
| Bleb extent at 6 mon | ||||||
| Model 1 | 0.902 | 0.683-1.190 | 0.464 | 0.439 | 0.276-0.700 | 0.001* |
| Model 2 | 0.923 | 0.697-1.222 | 0.574 | 0.362 | 0.215-0.607 | <0.001* |
| Model 3 | 0.934 | 0.701-1.245 | 0.640 | 0.351 | 0.205-0.601 | <0.001* |
Table 4
Univariate and multivariate Cox HRs of filtering bleb size for complete success according to bleb size
| Risk factor (n = 145) | Complete success | |||
|---|---|---|---|---|
|
|
||||
| Univariate analysis | Multivariate analysis | |||
|
|
|
|||
| HR (95% CI) | p-value | HR (95% CI) | p-value | |
| Filtering bleb height ≥2CCT (n = 91) | 0.840 (0.587-1.203) | 0.342 | 0.893 (0.591-1.348) | 0.719 |
| Filtering bleb extent ≥2Q (n = 54) | 0.461 (0.345-0.704) | <0.001* | 0.461 (0.306-0.695) | <0.001* |
Table 5
Univariate and multivariate Cox HRs of filtering bleb size for qualified success according to bleb size
| Risk factor (n = 145) | Qualified success | |||
|---|---|---|---|---|
|
|
||||
| Univariate analysis | Multivariate analysis | |||
|
|
|
|||
| HR (95% CI) | p-value | HR (95% CI) | p-value | |
| Filtering bleb height ≥2CCT (n = 91) | 1.111 (0.639-1.931) | 0.451 | 1.291 (0.665-2.506) | 0.451 |
| Filtering bleb extent ≥2Q (n = 54) | 0.541 (0.290-1.010) | 0.020* | 0.453 (0.232-0.884) | 0.020* |
- TOOLS



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Supplement1
Supplement1 Print
Print




