Protective Role of 360° Laser Retinopexy in Patients with Rhegmatogenous Retinal Detachment: a Systematic Review and Meta-analysis
Article information
Abstract
Purpose
Visual impairment from retinal re-detachment could be debilitating. The aim of this review is to evaluate the role of 360° laser retinopexy on success rate of rhegmatogenous retinal detachment (RRD) repair by a meta-analysis study.
Methods
The PubMed, Scopus, and the Cochrane Library databases were searched comprehensively from the date of database inception to January 2021, evaluating the role of 360° laser retinopexy in visual and anatomical success rate of RRD repair. This review was conducted based on the preferred reporting items for systematic review and meta-analysis (PRISMA) protocols.
Results
Among 202 articles screened for eligibility, six studies were found to be eligible for inclusion in our final analysis. Our meta-analysis demonstrates that prophylactic treatment with circumferential laser photocoagulation has no significant effect on the initial rate of retinal re-detachment or final best-corrected visual acuity following pars plana vitrectomy repair of RRD. Subgroup analysis of studies (n = 3) with 23-gauge pars plana vitrectomy, however, favors attachment rate in patients undergoing 360° prophylactic laser treatment.
Conclusions
Three hundred and sixty degree laser retinopexy appears to have favorable outcomes in patients undergoing 23-gauge retinal detachment repair. This protective effect, however, is not apparent with inclusion of 20-gauge vitrectomy studies.
Rhegmatogenous retinal detachment (RRD) is a sight-threatening condition that is caused by the presence of full-thickness retinal breaks with subsequent accumulation of liquefied vitreous in between the neurosensory retina and retinal pigment epithelium [1]. As a consequence of retinal detachment and its extension into the macula, there could be a significant decline in vision due to the rapid loss of photoreceptors [2,3]. Hence, prompt and successful treatment of RRD is essential for improved visual prognosis [4,5].
At present, pars plana vitrectomy (PPV) is growing in popularity for repair of RRD and yet, traction on the vitreous base is thought to contribute to the development of new peripheral breaks that might lead to surgical failure. In particular, the crystalline lens can impede access to peripheral retina in cases of phakic patients [6,7]. As a potential solution, a proposed technique that is routinely practiced by some retinal surgeons includes application of 360° laser retinopexy to the peripheral retina for enhanced success rate of surgical repair. Presumably, application of circumferential laser creates a chorioretinal scar that might cover any missed breaks and wall off subretinal fluid conduits from the anterior to the posterior retina. Here we performed a meta-analysis of randomized and retrospective studies to investigate the effects of 360° laser retinopexy versus localized laser in areas of retinal breaks on the attachment rate and final visual outcome of patients undergoing RRD repair by the PPV technique.
Materials and Methods
This study is conducted in accordance with widely accepted preferred reporting items for systematic review and meta-analysis (PRISMA) guidelines [8]. To avoid bias, each stage of the study is carried out by two researchers independently (SB and CS) and in case of disagreement that could not get resolved by discussion, a third reviewer (EC) is consulted. This meta-analysis project is classified as exempt by the office of the institutional review board.
Search strategy and selection criteria
PubMed, Scopus, and the Cochrane Library were searched from the date of inception of the databases to January 2021 using the following search keywords: (“retinal detachment” OR [detachment AND retina]) AND (laser OR photocoagulation OR retinopexy) AND (360 OR “three hundred and sixty” OR circumferential). Noted one more issue.
Inclusion criteria were 1) patients with RRD that have undergone repair by the PPV with either localized laser photocoagulation or 360° laser retinopexy and 2) primary outcome assessment with attachment rate and best-corrected visual acuity (BCVA) after the initial surgical repair. Exclusion criteria included 1) non-English articles, 2) failure to locate retinal breaks, 3) proliferative vitreoretinopathy (PVR) of grade C or higher, 4) cases series associated with complicated causes of retinal detachment such as infections or other inherited disorders, 5) detachment after silicone oil removal, and 6) application of retinectomy during the surgical repair. Combination of PPV with phacoemulsification or scleral buckle was not considered as exclusion factors. Two authors (SB and CS) independently reviewed each title and/or abstract and eliminated studies based on the eligibility criteria, after which the full text of each article was reviewed.
Data extraction and quality assessment
The selected articles were used to extract information on the first author, publication date, study design, intervention and sample size, rate of retinal attachment, BCVA, and follow up periods. The quality of randomized studies was assessed using the Cochrane Collaboration’s tool [9], assigning grades of high, unclear, and low risk of bias across the following domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias [10].
Statistical analysis
The RevMan software ver. 5.4 (Cochrane Collaboration, Copenhagen, Denmark) was used to assess continuous variable outcomes of BCVA and dichotomous outcomes of attachment rate using the weighted mean difference and odd’s ratio, respectively. Overall effect size with 95% confidence interval was calculated using a random model. The heterogeneity of studies was accessed using the chi-square test based on the I2 values for each pooled estimate (p < 0.10 represents significant heterogeneity). A forest plot was created using the same software (p < 0.05 was considered statistically significant). Egger’s and Begg’s tests were not performed due to a small number of selected studies.
Results
Search results
In this study, among 202 articles screened for eligibility, 175 non-duplicate articles were identified, 150 of which were excluded after the title and abstract screen. After review of the full text of the remaining articles, 19 additional articles are eliminated due to the lack of necessary criteria. Therefore, a total of six qualified studies were used for qualitative assessment to address the role of 360° barrier laser on attachment rate (three retrospective, three randomized) and BCVA (two retrospective, two randomized) of patients undergoing RRD repair by the PPV technique. Fig. 1 depicts the flow chart of literature screening and selection, while Table 1 demonstrates the characteristics of each selected study [11–16].
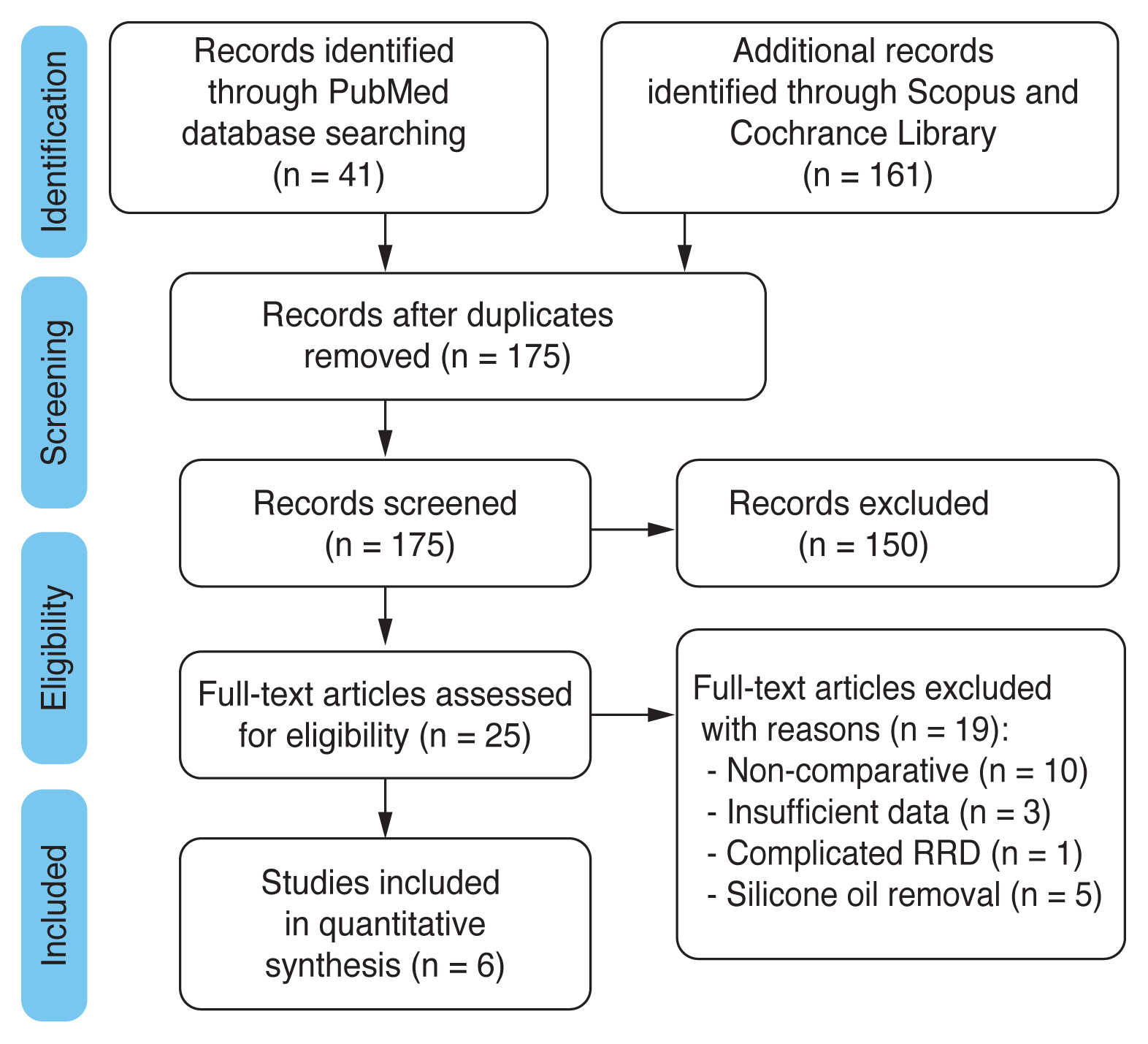
Preferred reporting items for systematic review and meta-analysis (PRISMA) flow chart of literature review. RRD = rhegmatogenous retinal detachment.
Study bias
Using the Cochrane Collaboration’s tool, the methodological quality of the randomized studies included in this review is demonstrated in Fig. 2. Two of the selected studies used standardized random allocation techniques, versus Bilgin et al. [11] that has employed randomization by patient’s order. Falkner-Radler et al. [13] reports masking of data assessors, while reporting a possible bias on selection of tamponade. Likewise, Falkner-Radler’s study is further biased by comparing PPV with 360° barrier laser to PPV with SB and localized laser. For other studies, it is unclear whether the outcome assessment or tamponade selection was a masked process. The publication bias testing via Egger’s and Begg’s tests was not carried out due to a relatively small number of selected studies.
Effectiveness of treatments
For our qualitative assessment, we have analyzed the protective roles of 360° laser in randomized studies versus all combined studies (randomized and retrospective) in patients undergoing active repair of RRD. The former approach reduces the risk of bias while the latter approach has a larger sample size with increased power of the analysis. Both analytic approaches yielded similar results as shown in Fig. 3. In comparison to localized retinopexy, application of prophylactic 360° laser does not reduce the risk of retinal detachment with p-values of 0.37 and 0.08 for randomized (n = 3 studies, 203 participants) and combined (n = 6 studies, 2,980 participants) studies, respectively. Likewise, the final BCVA did not differ between either group, with p-values of 0.41 and 0.56 for randomized (n = 2 studies, 153 participants) and combined studies (n = 4 studies, 2,779 participants), respectively. Subgroup analysis of patients undergoing 23-gauge PPV (n = 3 studies, 293 participants), however, demonstrates favorable outcomes in attachment rate of patients receiving 360° prophylactic laser treatment, as shown in Fig. 4 with p-value of 0.02.
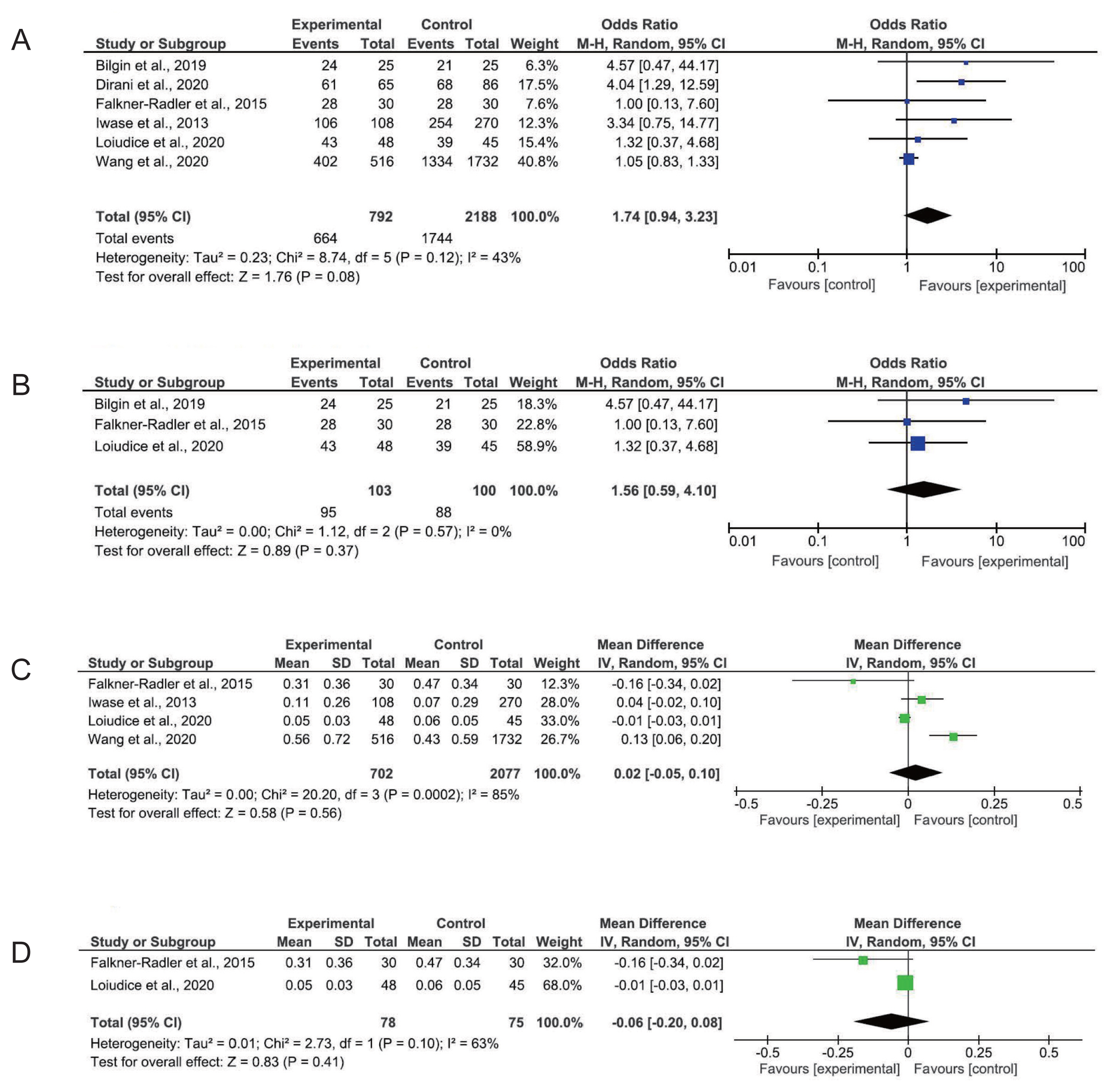
Forest plot of the effects of 360° laser retinopexy (“Experimental”) versus localized laser (“Control”) on initial rate of retinal attachment and best-corrected visual acuity (BCVA) in patients undergoing repair of a rhegmatogenous retinal detachment. (A) Attachment rate in all studies, (B) attachment rate in randomized studies, (C) BCVA in all studies, and (D) BCVA in randomized studies. M-H = Mantel-Haenszel; CI = confidence interval; SD = standard deviation; IV = inverse variance; Random = random-effect model.

Sub-group Forest plot of the effects of 360° laser retinopexy (“Experimental”) versus localized laser (“Control”) on initial rate of retinal attachment in patients undergoing repair of a rhegmatogenous retinal detachment with 23-gauge pars plana vitrectomy. M-H = Mantel-Haenszel; CI = confidence interval.
It is worth noting that, except for combined analysis of final BCVA (Fig. 3C), the heterogeneity p-values for all analyses were equal or more than 0.1, indicating consistency in the reported outcome of selected studies.
Discussion
Vitreoretinal traction caused by vitreous adhesion is an important factor in development of RRD via formation of retinal breaks as well as a tractional force that makes subretinal space accessible for passage of vitreous fluid [1,17]. Therefore, surgical interventions including PPV, scleral buckling (SB), or combination of these techniques are generally directed at relief of vitreoretinal traction, sealing of breaks by chorioretinal scars, and in most cases, drainage of subretinal fluid [18]. In particular, SB is an excellent technique for relief of vitreous traction via indentation of the eye wall. Furthermore, scleral buckle success in treatment of RRD is attributed to enhancing the proximity of retinal pigment epithelium and detached retina by displacement of subretinal fluid while closing the breaks that permit fluid into the subretinal space [19,20]. Nevertheless, there is low evidence to indicate that there may be any difference between PPV and SB in terms of final anatomical success or visual gain [21]. In addition, there are post-operative complications associated with SB such as refractive change, strabismus and diplopia, globe ischemia, buckle extrusion, and serous choroidal detachment that might encourage some retinal surgeons to choose PPV technique over SB [22]. On the other hand, despite its popularity, the PPV technique also has limitations including difficulties in overcoming vitreoretinal tractional forces at the vitreous base, particularly in phakic patients with a crystalline lens that could impede access to the peripheral vitreous [6,7]. It is recommended by many surgeons to carefully shave peripheral vitreous as new breaks are thought to be caused from traction at the vitreous base [23,24]. At the same time, shaving the peripheral vitreous remains an area of controversy by other investigators who suggest a comparable success rates without the use of scleral-depressed vitreous base shaving [25].
Development of PVR, failure to locate all the retinal breaks, and creation of new breaks from vitreous base traction remain as major causes of retinal re-detachment [7]. To overcome the latter issues, application of peripheral retinopexy is proposed for enhanced success of RRD repair, analogous to creation of a second ora serrata [24,26]. Nevertheless, controversy remains regarding the effectiveness of 360° prophylactic laser retinopexy in patients with RRD, for which we have performed the current meta-analysis study.
A key strength of this study includes inclusion of multiple randomized as well as retrospective studies with separate analyses provided for randomized trials (for low risk of bias) versus all studies combined (for larger sample size and power of analysis). In our study, we evaluated three randomized clinical trials and three retrospective studies that met our search criteria on the effect of peripheral barrier laser in protection against re-detachment in patients with RRD. Analysis of randomized studies alone, or all studies combined came up with the same conclusion that 360° laser retinopexy does not influence the initial attachment rate or final BCVA of patients that undergo RRD repair by a PPV technique. Nevertheless, three of these studies use 20-gauge vitrectomy approach, two of which also combine PPV with the SB technique, which could further enhance bias in analysis of the results. Indeed, exclusion of these studies with subgroup analysis of patients undergoing 23-gauge PPV alone demonstrates that attachment rate was significantly higher upon application of 360° Prophylactic laser. Hence, it appears that in the absence of scleral buckle, application of circumferential barrier laser with modern vitrectomy techniques, namely 23-gauge and potentially smaller gauge vitrectomy instruments, provides a protective role against re-detachment following initial repair of a RRD. It is worth noting that for patients that had a successful repair, intraoperative or postoperative application of prophylactic circumferential laser also protected against future recurrence of detachment after removal of the silicone oil, as concluded by He et al.’ meta-analysis review [27].
Potential limitations of retrospective studies include bias towards the use of prophylactic circumferential laser treatment, scleral buckle, or type of tamponade selected pending severity of RRDs. Another limitation is a relatively small number of participants in most reported cases resulting in lower power of the analysis, though our meta-analysis evidence level remains higher in comparison to the individual reports. Lastly, this meta-analysis was conducted on aggregate data rather than individual participants, which is considered more accurate than the former analysis [28].
In conclusion, in comparison to localized laser photocoagulation, prophylactic 360° laser retinopexy enhances attachment rate in patients undergoing RRD repair with the 23-gauge PPV technique. Likewise, in patients with prior successful RRD repair, circumferential laser protects against re-detachment after removal of the silicone oil [27]. Furthermore, patients with undetected retinal breaks might also benefit from this treatment modality [29]. Nonetheless, in spite of all these protective effects, considerations should be made regarding the potential adverse effects of this prophylactic treatment including postoperative development of tonic pupil and loss of corneal sensitivity with consequent risk of neurotrophic ulcers [30,31].
Notes
No potential conflict of interest relevant to this article was reported.

