Dear Editor,
Since traumatic macular hole (TMH) was first described in 1869, there have been hypotheses to explain its pathophysiology and MH closure. Previously suggested mechanisms for macular hole (MH) closure were glial or retinal pigment epithelium (RPE) cell proliferation [1], contraction of the epiretinal membrane or operculum around the edge [2,3].
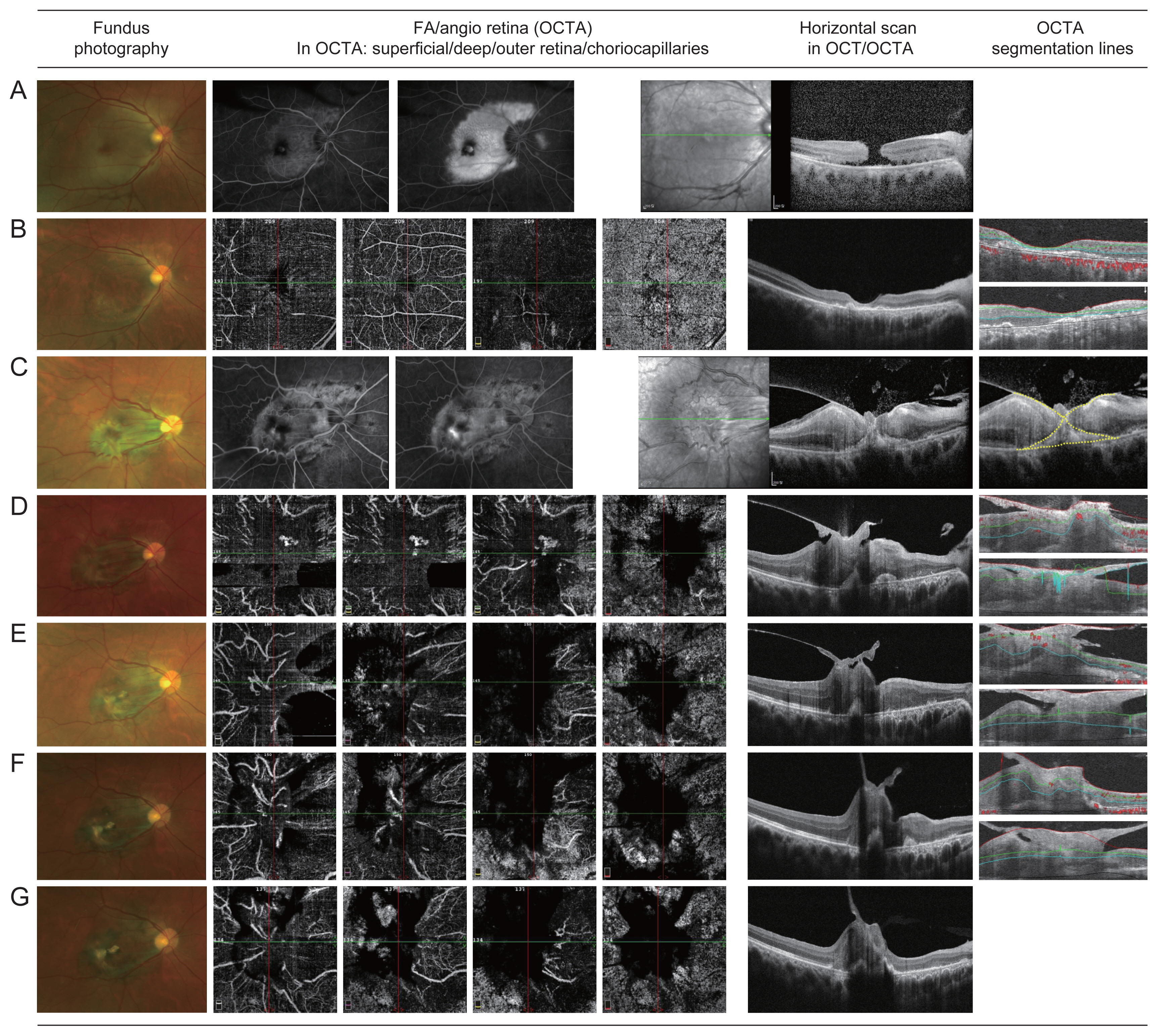
Recently, we experienced a spontaneously closed TMH accompanied by macular choriovitreal membrane (MCVM) formation in a young patient. A 34-year-old man without significant medical history was admitted to the emergency room with decreased vision in his right eye after being hit by a baseball one day previously. His best-corrected visual acuity (BCVA) was 20 / 400 and he underwent fundus photography, spectral-domain optical coherence tomography (OCT), and fluorescein angiography (FA). On evaluation, full-thickness MH on OCT and FA showed diffuse hyperfluorescence with window defects on the macula (Fig. 1A). As there were no signs of choroidal rupture like subretinal hemorrhage or disruption of the BruchŌĆÖs membrane, we diagnosed as a TMH without choroidal rupture. In addition, due to the hyperfluorescent lesion being associated with the commotio retinae in the FA, we planned to perform OCT angiography (OCTA) during follow-up to check the occurrence of secondary choroidal neovascularization (CNV). Two weeks after the injury (Fig. 1B), his BCVA slightly improved to 20 / 320, and OCTA showed a spontaneously closed MH with focal RPE disruption. One month later (Fig. 1C), spectral-domain OCT revealed MCVM formation. MCVM is a subfoveal choroidal fibrovascular strand penetrating the surface of the inner retina and growing as an epiretinal fibrovascular membrane accompanied by vitreomacular traction (VMT) (Fig. 1C, yellow dotted line). In addition, FA showed persistent hyperfluorescence with pinpoint foveal leakage similar to CNV. On the subsequent monthly follow-up, MCVM traction and foveal vascular congestion with neovascular network were noted in OCTA. Despite these anatomical changes, his BCVA remained the same at 20 / 400 (Fig. 1D, 1E). Intravitreal anti-vascular endothelial growth factor injection for macular edema was not administered because it was considered to have no functional benefit for the following reasons. First, extensive macular ischemia due to trauma (Fig. 1A), and RPE changes in this region were observed after 1 month (Fig. 1C). Second, the closure of the TMH was due to MCVM formation rather than rearrangement of the retinal tissue, which resulted in little change in visual acuity, even after the macular deformation with increased traction. In terms of VMT, vitrectomy was to be considered if the traction had worsened. After 6 months of follow-up (Fig. 1F), his BCVA slightly improved to 20 / 200 and regressed vascular congestion with remaining MCVM traction was observed. At the 1-year follow-up (Fig. 1G), his vision remained constant, and regression of VMT with vascular congestion was in progress without intervention.
In this study, we found that OCTA is a noninvasive and effective imaging technique for repeated examinations of chorioretinal changes in MH, as reported in previous studies [4]. Compared with idiopathic MH, automated segmentation is inaccurate because of the artifacts of traction membranes on the retinal surface [5]. However, once manual segmentation was performed, the intraretinal capillary plexus and neovascular network could be sufficiently visualized. Among several suggested mechanisms for the formation and closure of MH, this case may be interesting evidence to support the hypothesis of glial or RPE cell proliferation filling the hole [1]. In this process, it could be seen that the high cellular proliferation of the patientŌĆÖs young age resulted in excessive fibrovascular proliferation. Since it has not been histologically confirmed whether the MCVM consists of glial or RPE cell origins, our hypothesis remains at the theoretical level. If the VMT worsens and vitrectomy is performed during a subsequent follow-up, histologic verification of the MCVM will be required. However, unlike idiopathic MH cases, in cases of severe macular ischemic damage after trauma and TMH closure by MCVM, the therapeutic benefit of anti-vascular endothelial growth factor injections or surgical treatments should be carefully considered.
To the best of our knowledge, this is the first report of MCVM formation with CNV after spontaneous closure of TMH. In addition, we were able to confirm that OCTA can be an effective tool to localize CNV, even under thick VMT.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






