Dear Editor,
Endophthalmitis is a sight-threatening condition that requires immediate attention. In general, patients are treated emergently with a vitreous tap for culture and gram staining followed by injection of intravitreal antibiotics (e.g., 0.1 mL of vancomycin 10 mg/mL, 0.1 mL of ceftazidime 22.5 mg/mL) [1,2]. Likewise, vitrectomy could be considered for enhanced visual outcomes in certain patients, namely those cases that are complicated by virulent pathogens, marked vitreous opacity, retinal detachment and poor initial visual acuity [3,4]. Nevertheless, vitreous and lens opacification in phakic patients could significantly hinder vitreous and fundus visualization, as a consequence of which performance of vitrectomy may pose a risk of damaging internal ocular structures such as the retina and posterior lens capsule. Here we propose a simple but novel technique that reduces the risk of damaging internal ocular structures via enhanced localization of the vitrectomy port in the vitreous cavity.
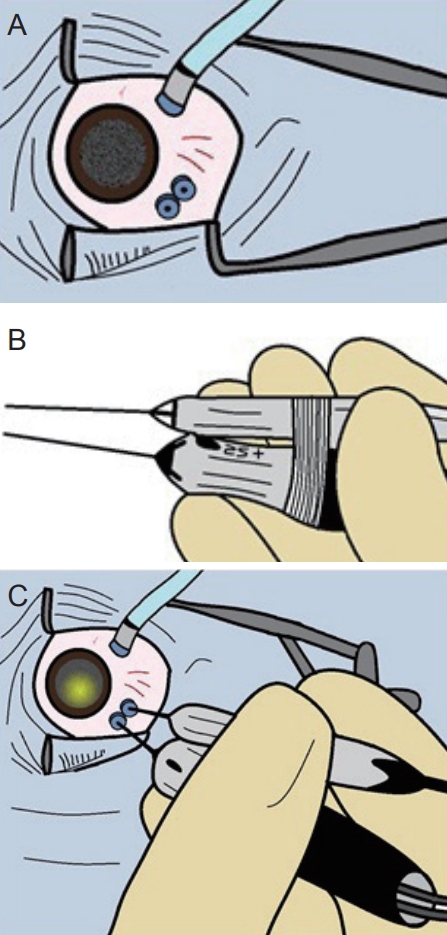
As a general setup for vitrectomy surgery by Alcon Constellation machine (Alcon Laboratories, Fort Worth, TX, USA), a 25-gauge infusion cannula is placed 3.5mm from the corneal limbus in the inferotemporal area. Under normal circumstances, the other two cannulas would be inserted superior to 3 and 9 oŌĆÖclock positions. For our new setup, however, only one of the cannulas is placed slightly superior to either 3 or 9 oŌĆÖclock positions, while the second cannula is inserted superior and as proximal as possible to the former cannula (Fig. 1A). Note that the temporal or nasal location of insertions is interchangeable pending the hand dominance laterality and/or comfort level of the surgeon. In the next step, the vitrectomy port and light pipe are taped together via steri-strips in a manner that both tips end at the same length (Fig. 1B). Using this set up, the taped instruments are held in one hand similar to a ŌĆ£chopstickŌĆØ and inserted into the vitreous via the two proximal cannulas as illustrated in Fig. 1C. Vitrectomy is then performed by holding the taped instruments in one hand, leaving the other hand free for any other necessary maneuvers such as scleral depression independent of an assist. It is worth noting that for this technique, the steri-strips were able to hold the two instruments together sturdily and the surgeonŌĆÖs hand did not get tired by holding the two instruments together, most likely due to the short duration of these operations.
Using this setup, our retina surgeons can more confidently gauge the location of vitrectomy port upon visualization of the light pipe, in that the two instruments are of the same length and only a few millimeters apart. The case shown in the video is a patient with endogenous methicillin-resistant Staphylococcus aureus infection that has presented to the emergency department with a combination of endophthalmitis and orbital cellulitis. Under these circumstances, one option is to consider removal of the phakic lens and fibrotic membranes to enhance the view, though these additional procedures could add further complications such as the risk of retained lens material, retinal tears and detachment, as well as extended length of the surgery. Hence, the ŌĆ£chopstickŌĆØ technique provides flexibility for performing vitrectomy without the need to manipulate the lens, while maintaining the second hand free for any additional maneuvers that are deemed necessary by the surgeon. The limitation of this technique, however, is reduced ability to control ocular movements due to the presence of both ports on the same side. Nevertheless, this limitation might not be of much issue in patients with endophthalmitis in that the general goal of surgery is to perform core rather than peripheral vitrectomy.
It is worth noting that a similar set up was described by Chalam et al. [5], where a fiber optic endoilluminator (0.5 mm) is secured to the curved 25-gauge vitrector (0.5 mm) for removal of subsclerotomy vitreous. In comparison, our approach eliminates the need for any additional preparations or costs, in that AlconŌĆÖs Constellation general vitrectomy instruments can be used to carry out the procedure. Furthermore, the width of instruments remains unchanged using the ŌĆ£chopstickŌĆØ technique, eliminating the need for larger sclerotomies. Hence, when the posterior view is limited, the ŌĆ£chopstickŌĆØ technique provides retina surgeons an alternative approach to perform vitrectomy in cases of severe endophthalmitis.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






