Dramatic Decrease in Ocular Deviation 1 Day before Surgery in Patients with Intermittent Exotropia
Article information
Abstract
Purpose
To evaluate the clinical characteristics of patients with intermittent exotropia who exhibited a dramatic decrease in ocular deviation 1 day before surgery.
Methods
This study retrospectively enrolled patients with intermittent exotropia who underwent surgery between December 2013 and December 2019. Those who exhibited a decrease in ocular alignment ≥10 prism diopters (PD) at the last examination (1 day before surgery) compared with the largest previous angle of deviation were included. A monocular occlusion test was performed to re-confirm the largest angle of ocular deviation.
Results
Among 547 patients with intermittent exotropia, 10 (six females; mean age, 8.6 years) exhibited a dramatic decrease in ocular deviation before impending surgery. The mean largest angle of deviation was 31.0 PD (range, 20 to 50 PD) at distance and 34.5 PD (range, 20 to 55 PD) at near. The mean control scores using the LACTOSE (Look and Cover then Ten Seconds of Observation Scale for Exotropia) scoring system were 2.5 at distance, 1.8 at near, and 4.3 when combined. Mean ocular deviation prior to the impending surgery decreased to 7.4 PD (range, 0 to 10 PD) at distance and 6.2 PD (range, -10 to 10 PD) at near. The largest angle of ocular deviation was re-confirmed using the monocular occlusion test in all patients. All patients underwent surgery as planned, and none exhibited postoperative overcorrection.
Conclusions
A relatively small number of patients with intermittent exotropia exhibited a dramatic decrease in ocular alignment 1 day before surgery but demonstrated a relatively better level of control. The monocular occlusion test was helpful in re-confirming the largest angle of ocular deviation.
The angle of ocular deviation can be variable according to level of control as measured during follow-up examinations in patients with intermittent exotropia [1,2]. Determining the largest angle of ocular deviation and designating it as the target for surgery is necessary to achieve favorable surgical outcomes in patients with intermittent exotropia [1,3,4]. Therefore, alternative methods, such as the monocular occlusion test, repeated measurements, and outdoor measurement, have been used to reveal the largest angle of ocular deviation [1].
The level of control in patients with intermittent exotropia can be affected not only by extrinsic factors, but also by intrinsic factors such as general health, alertness, attention span, and level of anxiety [5]. Pediatric patients scheduled to undergo anesthesia and surgery usually report significant anxiety [6,7]. Although rare, a dramatic decrease in ocular deviation caused by anxiety associated with impending surgery can also occur in patients with intermittent exotropia [5]. It is recommended to perform the surgery as planned; however, the risks for postoperative overcorrection should be considered by even the most experienced surgeons [5]. To our knowledge, no previous studies have investigated the characteristics of patients who exhibit a dramatic decrease in ocular deviation preoperatively. Accordingly, we examined patients with intermittent exotropia who exhibited a dramatic decrease in ocular deviation 1 day before their scheduled surgery.
Materials and Methods
The present study adhered to the tenets of the Declaration of Helsinki and was approved by the institutional review board of Yeungnam University Hospital (2019-12-045). Given the retrospective nature of the study and the use of anonymized patient data, requirements for informed consent were waived by the board. This study retrospectively enrolled patients with intermittent exotropia who underwent surgical treatment between December 2013 and December 2019. Patients with intermittent exotropia who exhibited a decrease in ocular alignment ≥10 prism diopters (PD) at both distant and near fixation compared with the largest angle of deviation at the last examination (1 day before surgery) were included in the study. Individuals with any other types of strabismus, such as oblique muscle dysfunction, dissociated vertical deviation, an A-V pattern, or nystagmus, were excluded. Individuals who had undergone previous intraocular surgery and those with any neurological impairment or severe unilateral amblyopia were also excluded.
Preoperative evaluation
At the initial visit, all patients underwent a full ophthalmologic examination, including testing of visual acuity and ocular alignment status, assessment of level of control, slitlamp biomicroscopy, refraction, fundus examination, and stereoacuity testing. Best-corrected visual acuity was measured, when possible. If patients were considered too young for optotype testing at the initial visit, visual acuity was evaluated based on fixation preference. The angle of deviation was measured both pre- and postoperatively using an alternate prism cover test at 6-m and 33-cm fixation in cooperative patients. An ocular patch was provided to the patients at the first visit, and they were instructed to occlude the non-dominant eye for 1 hour at the next visit to measure the largest angle of deviation. The level of control was assessed using the Look and Cover then Ten Seconds of Observation Scale for Exotropia (LACTOSE) control scoring system [8]. This control system was developed by incorporating scales for both distance and near evaluations (5-point scales, scored from 0 to 4 each), yielding a total score ranging from 0 to 8. A higher score indicates a poorer level of control. Controllability was defined as the patient’s subjective awareness of exotropia or diplopia associated with presence of exotropia and ability to instinctively correct ocular deviation. More than two preoperative examinations were performed on each patient before surgery. Stereoacuity measurements were carried out using the Lang I (Lang-Stereotest AG, Küsnacht, Switzerland) and Stereo Fly Stereotest (Stereo Optical, Chicago, IL, USA) when the patient was able to cooperate and complete the test.
Final examination of ocular alignment before surgery
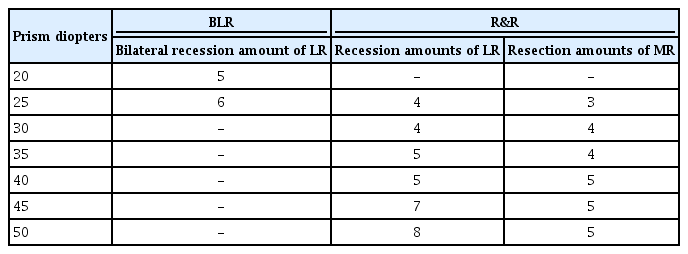
Patients were admitted to the hospital 1 day before surgery according to the authors’ preoperative protocol. The final examination of ocular alignment was performed on the evening before surgery (usually between 6:00 and 7:00 p.m.). If any patients exhibited a dramatic decrease in ocular deviation compared with the largest angle obtained during previous measurements, a 30-minute monocular occlusion test was conducted to confirm the largest ocular deviation. Additionally, a 1-hour monocular occlusion test was performed if the 30-minute monocular occlusion test failed to reveal the largest ocular deviation. All measurements of ocular deviation were performed by the same clinician (WJK). The surgery was carried out using the surgical protocol developed at the authors’ clinic (Table 1). The angle of deviation measured during the first follow-up visit within 1 week of surgery was defined as the immediate postoperative deviation. The patients were followed-up at 1, 3, 6, and 12 months after the surgery and then every 6 months thereafter.
Statistical analysis
Continuous data are expressed as mean with standard deviation, and categorical data are shown as count and percentage. Patient data, including sex, age at surgery, largest angle of ocular deviation, level of control, controllability, decrease in ocular deviation at the final examination, and surgical outcomes, were collected. Data were analyzed using the IBM SPSS Statistics ver. 20.0 (IBM Corp., Armonk, NY, USA).
Results
Basic characteristics of patients with intermittent exotropia
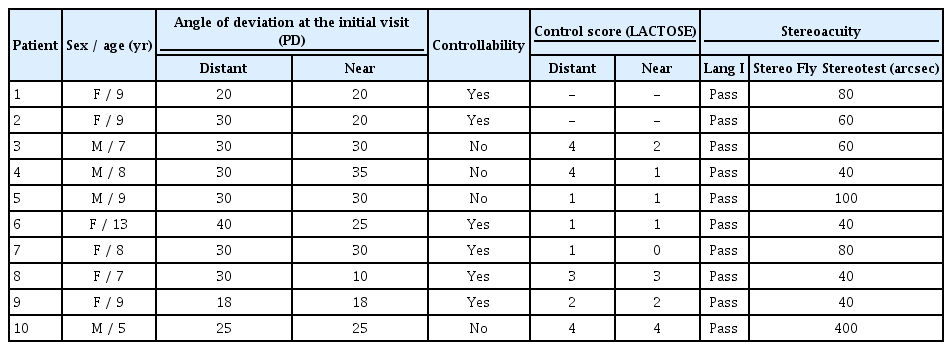
This study retrospectively reviewed 547 patients with intermittent exotropia who underwent surgical treatment during the study period. Among these participants, 10 (6 females) exhibited a decrease in ocular alignment ≥10 PD compared with the largest angle of deviation obtained at the last examination (1.8%, 10 / 547). The basic characteristics of the included patients are shown in Table 2. The mean age of the included patients was 8.5 ± 2.1 years (range, 5 to 13 years). Eight patients had basic type of intermittent exotropia. Two patients (patients 6 and 8) demonstrated pseudo-divergence excess type of intermittent exotropia. The level of control achieved as assessed using the LACTOSE scoring system was measured for eight included patients. The mean control scores were 2.5 ± 1.4 at distant fixation, 1.8 ± 1.3 at near fixation, and 4.3 ± 2.4 when combined. Six patients (60.0%, 6 / 10) exhibited controllability of exotropia. The mean spherical equivalent refractive errors of the included patients were -0.59 ± 1.12 diopters (D; range, -2.25 to +1.00) in the right eye and -0.65 ± 1.02 PD (range, -2.00 to +1.00) in the left eye.
Decrease in ocular deviation 1 day before surgery and the effect of the monocular occlusion test
The largest angles of ocular deviation, initial ocular deviation at the final examination, and ocular deviation 1 day before surgery are summarized in Table 3. The mean largest angle of deviation was 31.0 ± 9.1 PD (range, 20 to 50 PD) at distant fixation and 34.5 ± 10.1 PD (range, 20 to 55 PD) at near fixation. The mean angle of ocular deviation decreased to 7.4 ± 5.6 PD (range, 0 to 16 PD) at distant fixation and 6.2 ± 8.4 PD (range, -10 to 16 PD) at near fixation 1 day before surgery. The largest decrease in ocular deviation was 50 PD at distance and 65 PD at near.
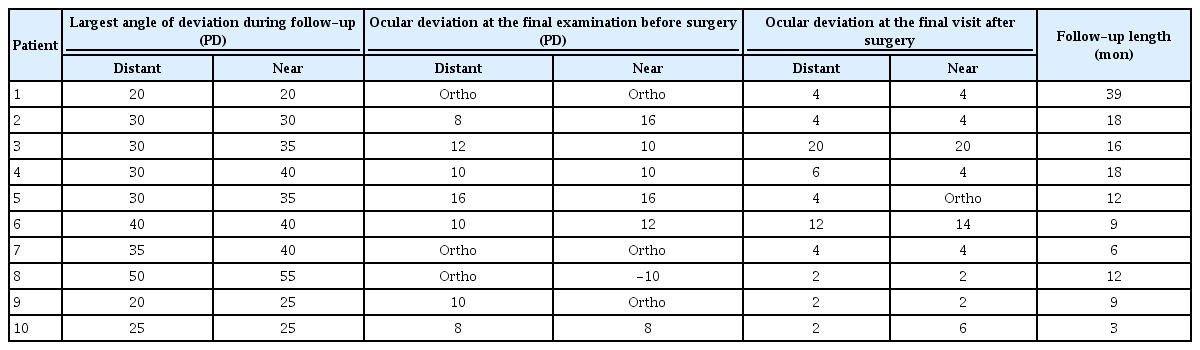
Clinical features of patients with intermittent exotropia who exhibited dramatic decrease in ocular deviation 1 day before surgery
The 30-minute monocular occlusion test was performed in all patients to re-check the largest angle of deviation, with nine patients exhibiting an increase in ocular deviation, the same number compared with the previous largest angle of ocular deviation. One patient (patient 8) who exhibited the largest decrease in ocular deviation required an additional 1-hour monocular occlusion test to confirm the largest ocular deviation. All patients underwent surgical treatment as planned. During postoperative follow-up examinations (range, 3 to 39 months), no patients exhibited postoperative overcorrection of exotropia.
Discussion
In the present study, 1.8% of all included patients with intermittent exotropia exhibited a dramatic decrease in ocular alignment ≥10 PD 1 day before surgery compared with the largest angle of deviation measured previously. These patients exhibited a relatively better level of control. Patients with controllability demonstrated a higher possibility of dramatic decreases in ocular alignment prior to an impending surgery. The monocular occlusion test was helpful in re-confirming the largest angle of ocular deviation. The surgery could therefore continue as planned without concerns about postoperative overcorrection.
Patients with intermittent exotropia may exhibit variable degrees of ocular deviation according to level of control during follow-up. A previous study demonstrated that more than half of patients with intermittent exotropia (62.8%, 216 / 344) exhibit variable angles of deviation during preoperative measurements [2]. von Noorden and Campos [5] described patients with intermittent exotropia who displayed a dramatic decrease in ocular deviation caused by anxiety associated with impending surgery. This anxiety may increase the level of patient control and lead to straight ocular alignment in patients with intermittent exotropia. It is recommended to perform the surgery as planned [5]; however, it sometimes may be difficult for the surgeon to decide on the best surgical strategy due to the possibility of postoperative overcorrection. No previous study has evaluated patients with intermittent exotropia who exhibited dramatic decreases in ocular deviation before impending surgery.
In the present study, a relatively small number of patients with intermittent exotropia exhibited a dramatic decrease in ocular deviation 1 day before surgery. These results are similar to those reported by Seo and Chung [9], who demonstrated that the angle of deviation at distance on the day of surgery was decreased in 1.9% (6 / 323) and the near angle was decreased in 6.8% (22 / 323) of patients. Patients who exhibited decreased near deviation were older than those with no change, and 81.8% of the patients were school-aged. Seo and Chung [9] postulated that older pediatric patients may be frightened by the prospect of surgery. In our study, the mean age of included patients was 8.5 years, which is old enough to be afraid of the prospect of surgery. Wariness of surgery may increase anxiety, which in turn leads to a temporal increase in level of control and a decrease in ocular deviation. One patient who exhibited the largest decrease in ocular deviation postponed the surgery one time due to extreme worry. She was also so anxious that she exhibited esotropia at near fixation at the last examination.
Patients with a relatively better level of control can exhibit dramatic changes in ocular deviation with impending surgery. In our study, the mean control score was lower, reflecting a better level of control compared with a previous study that included pediatric patients with intermittent exotropia [8]. The included patients showed good stereoacuity. Patients with relatively better fusional potential are considered more likely to maintain a period of normal ocular alignment but can easily mask the full amount of ocular deviation, leading to the observed dramatic decrease in ocular deviation [2]. More than one-half of included patients demonstrated controllability―a subjective awareness of exotropia. The level of control in patients with controllability may be more vulnerable to intrinsic factors such as anxiety. All examinations in the present study were performed by the same clinician in the same clinical settings, including fixation distance and accommodative targets. Therefore, the effect of extrinsic factors such as examiner, fixation distance, target size, and room luminance on the level of control should have had little influence on the results [5].
Based on our results, surgery can be performed in these patients as planned. Although patients with intermittent exotropia can exhibit a dramatic decrease in ocular deviation before surgery, spontaneous improvement of ocular deviation is rare in the natural course of intermittent exotropia [10,11]. We attempted to re-confirm the largest angle of ocular deviation using an alternate method, and the surgery was performed as planned. The study by Seo and Chung [9] demonstrated that the rate of postoperative overcorrection may be high in patients with decreased near deviation on the day of surgery. However, no patients in our study experienced postoperative overcorrection. We postulate that these differences can be attributed to differences in preferred surgical procedure and target of surgery. Previous studies only included patients who underwent bilateral lateral rectus recession. We performed the bilateral lateral rectus recession procedure or unilateral lateral rectus recession and medial rectus resection based on surgeon preference after re-confirmation of the largest angle of ocular deviation.
To re-confirm ocular alignment, a 30-minute monocular occlusion test was performed in all patients. The monocular occlusion test is used to differentiate the type of exotropia between true and pseudo-divergence excesses by blocking fusional stimuli and disruption of the tonic convergence [1]. Furthermore, this test can determine the largest ocular deviation in patients with intermittent exotropia. The 30-minute monocular occlusion test, which is less time-consuming than the hour-long method, was adequate for revealing the largest angle of ocular deviation, except in one patient. A 1-hour monocular occlusion test was required to re-confirm the largest angle of ocular deviation in this patient. Therefore, the 30-minute monocular occlusion test may be helpful in re-confirming the extent of ocular deviation in patients who exhibit a dramatic decrease in ocular deviation prior to surgery.
In addition to our results, methods to mitigate anxiety due to impending surgery should be considered for patients with intermittent exotropia. Although the level of control and amount of ocular deviation can be affected by anxiety associated with impending surgery, alternative methods of calming patients with anxiety have not been extensively studied in our field. Recently, a preoperative preparation program focusing on reducing anxiety before surgery was developed for pediatric patients [12,13]. The adaptation of this program and its effect on the angle of ocular deviation may be considered as a future topic of investigation.
The present study had several limitations. First, psychological test(s) to assess the degree of anxiety in our patients were not performed due to the retrospective nature of the study. Psychological tests that reflect an individual’s personality may be helpful in understanding the characteristics of patients who exhibit a dramatic decrease in ocular deviation before impending surgery. Second, the influence of parents on the patient anxiety was not considered in this study. Parental anxiety is strongly related to child preoperative anxiety and postoperative pain [14]. It is not uncommon for the parents of pediatric patients with preoperative anxiety to also be very anxious about the surgery. The effect of parental anxiety on pediatric patients with intermittent exotropia may be considered as a future topic of investigation.
Notes
No potential conflict of interest relevant to this article was reported.