Dear Editor,
Implants, the mainstay of treatment for repair of orbital wall fractures, restore the structure and function of the internal orbit. Inflammation and infections related to implants are common complications of orbital wall fracture repair. Most complications occur acutely, with immediate rejection occurring within the first few months after surgery. However, there have been a few reported cases of delayed infections that were cystic in form. Here, we present a case of delayed emphysema in the medial orbital wall of a patient who underwent repair 15 years previously. To our knowledge, this is the first case report of an encapsulated emphysema resulting from a delayed inflammatory reaction to a silastic sheet implant.
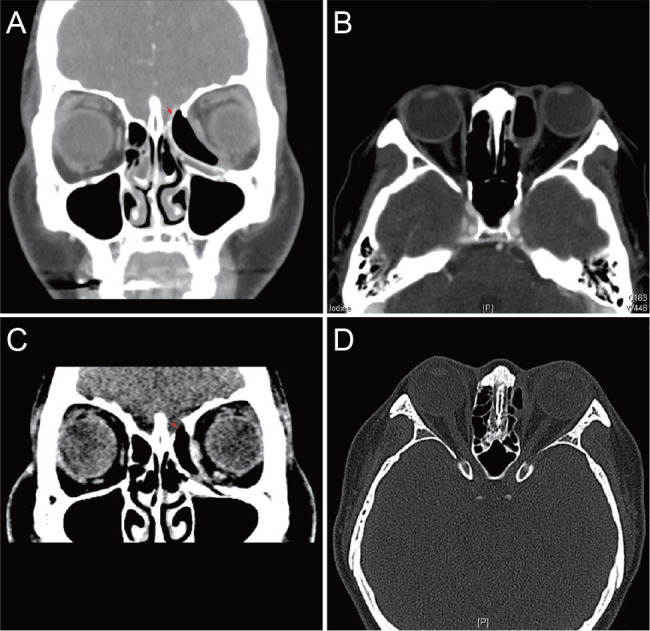
A 43-year-old female presented to our clinic complaining of recurrent swelling of the left medial canthal area for 3 years. Her past ocular history was remarkable for a traumatic left orbital wall fracture repair with a silastic sheet 15 years previously. Upon presentation, her best-corrected visual acuity was 20 / 20 in both eyes, and intraocular pressure was 14 mmHg in the right and 12 mmHg in the left. Hertel exophthalmometry was 14 mm on the right and 16 mm on the left with a base of 113 mm. Hess and the binocular single vision test showed no specific findings. No definite limitation of ocular motility or strabismus was noted in primary position. Furthermore, no signs of inflammation (heat sensation, redness, and tenderness) were noted. Computed tomography (CT) revealed an encapsulated emphysema surrounding a silastic sheet displaced into the ethmoid sinus, shifting the left eyeball temporally (Fig. 1A, 1B). The fovea ethmoidalis was severely eroded with suspicious extrusion of the silastic sheet. The patient underwent surgical removal of the implant with partial removal of the fibrous capsule through a transcaruncle and fornix approach. Intraoperative findings revealed an intact lacrimal sac and absence of cerebrospinal fluid leakage. Pathology of the capsule revealed granulation and fibrosis, and culture results were negative. We believe that a capsule formed around the silastic sheet, resulting in an airway connection to the sinus and allowed entrapment of air. A part of the fibrous capsule was intentionally left in place to prevent enophthalmos (Fig. 1C, 1D). Follow-up evaluation showed no complications, and a one-year postoperative CT scan revealed no significant findings. With good postoperative results, she was lost to follow-up.
To date, several alloplastic materials, such as silastic sheeting, titanium, and porous polyethylene, have been introduced. These materials eliminate donor site morbidity, reduce operative time, and are readily available. Silastic sheets have been favored in the past for their low cost, flexibility, and durability in large orbital fractures. However, post-operative complications, such as fibrous capsule formation, infection, and extrusion, have been reported. In such cases, silastic sheets can easily be removed due to absence of adhesion and vascularization. Nevertheless, surgical results using silastic sheets are controversial. Morrison et al. [1] reported that 13.2% of patients underwent implant removal due to infection, pain, extrusion, or diplopia. Yun et al. [2] reported that 4.3% of patients required implant removal within a mean of 23.3 months. Moon et al. [3] reported that the revision rate in groups using silastic plates was 5.4%, which was significantly higher than the rate for other materials. However, Prowse et al. [4] reported that the revision rate following use of silastic sheets was lower than that rate for non-silastic materials. Currently, our institute no longer uses silastic sheets for fracture reconstruction. Instead, titanium and porous polyethylene are used.
In the present case, swelling of the medial canthal area was the patient's only clinical symptom. The encapsulated emphysema caused displacement of the eyeball and thinning of the ethmoid roof, threatening extrusion into the cranial space. Capsule formation near the medial orbital wall is extremely dangerous and significantly increases the risk of infection due to anatomical proximity to the ethmoid sinus. We recommend a CT scan for all patients with history of wall fracture repair who present with symptoms of swelling despite absence of signs of inflammation. In our case, timely removal of the implant with partial removal of the fibrous capsule prevented severe complications. As new alloplastic materials emerge in clinical practice, the role of the ophthalmologist will become increasingly important for early recognition and timely management of unprecedented adverse events.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






