Importance of Head Position after Gas Tamponade in Bilateral Descemet's Membrane Detachment Following Cataract Surgery
Article information
Dear Editor,
Descemet's membrane detachment (DMD) is a rare complication of cataract surgery. It is associated with inadequate surgery techniques and pre-existing anatomical factors. Herein we present a case of bilateral extensive DMD that occurred after uneventful cataract surgery and suggest appropriate management for DMD resolution.
A 57-year-old woman was referred for refractory DMD after cataract surgery. According to her medical records, cataract surgery with phacoemulsification was completed without any complications but vision loss with diffuse DMD and marked corneal edema were detected on the first postoperative day (POD). Air injection into the anterior chamber in the supine position was performed twice for 2 weeks, but there was no improvement. Slit lamp examination and anterior optical coherence tomography revealed total DMD with severe corneal edema, and best-corrected visual acuity (BCVA) was finger-count/30 cm in her left eye. Fourteen percent C3F8 gas injection in a supine position was performed in her left eye 5 times. Two months postoperatively partial DMD remained but it had stabilized, and BCVA was 20 / 50 in her left eye.
Six months later, the patient requested cataract surgery on her right eye. In preoperative examination including specular microscopy, no anatomical problems were detected in her right eye. Routine cataract surgery with temporal clear corneal incision was performed gently without any complications by a skillful surgeon. On POD 1 day, BCVA was hand-motion and total DMD was detected in her right eye (Fig. 1A, 1B). Immediately, 14% C3F8 gas was injected into the anterior chamber in the supine position, but DMD remained stationery after gas injection was performed 3 times (Fig. 1C). On POD 6 days, the patient was instructed to maintain a left-decubitus position for tamponade at the temporal incision site after 14% C3F8 gas injection. One day later DMD recovered dramatically (Fig. 1D, 1E). Two weeks postoperatively the DMD was completely resolved and only the demarcation line was detected (Fig. 1F). Six months after surgery, her BCVA was 20 / 25 in the right eye.
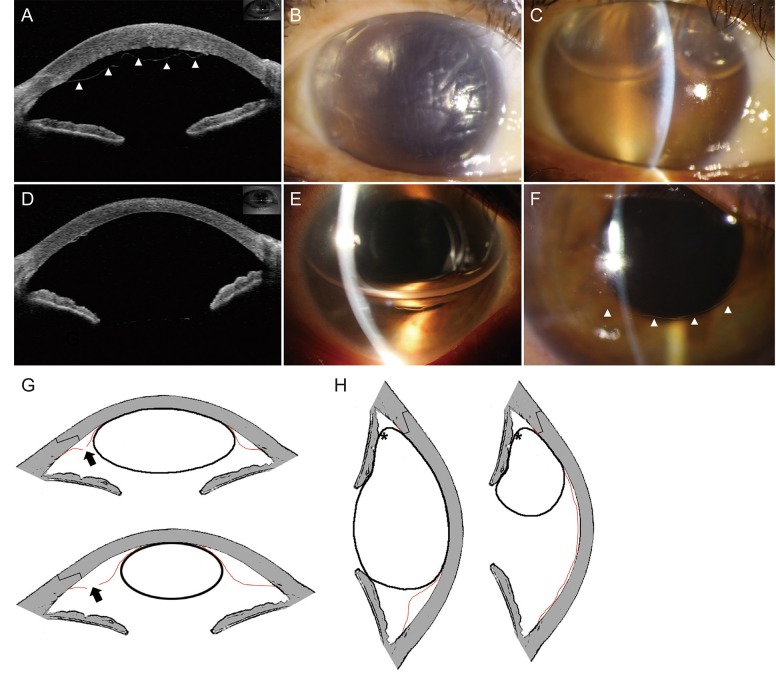
A comparison of supine and lateral decubitus position after gas tamponade. (A) Anterior optical coherence tomography revealed total Descemet's membrane detachment (DMD) (arrowheads). (B,C) Slit lamp photographs depicted extensive DMD, and DMD remained with gas bubbles. (D,E) DMD recovered dramatically the day after the left-decubitus position was adopted. (F) Only a small amount of DMD (arrowhead) was detected. (G) In the supine position, the bubble in the anterior chamber could not seal off the incision site and fluids could flow into the incision site (arrows). (H) In a decubitus position, the bubble sealed off the incision site more effectively, even when the bubble became smaller (stellates). The red demarcation line represents Descemet's membrane.
DMD is a rare complication of cataract surgery and most detachments at the incision site are small and usually resolve spontaneously or after a small number of gas injections, without significant visual consequences. In the present case, extensive bilateral DMD occurred after uneventful cataract surgery was performed by two skillful surgeons. Previous studies suggest that signs of abnormality in the fibrillary stromal attachment to Descemet's membrane may constitute a predisposition to bilateral DMD, but no clear underlying etiology of bilateral DMD has been determined [12]. In preoperative examination in the present case, neither slit-lamp nor specular microscopy indicated unhealthy endothelium.
In the current case of bilateral DMD, the outcomes in the right eye were more successful than those in the left eye with regard to both DMD resolution and visual acuity. We assume that the most critical factor related to these results is the head position after gas injection for tamponade at the Descemet's membrane break site. Because the temporal clear cornea was incised in the present case, the patient was instructed to lie in a left-decubitus position to maintain gas tamponade at the temporal incision site, and DMD recovered dramatically a day later. A key element of the procedure is sealing off the Descemet's membrane break to stop the influx of fluid through the break and gain time for the condition to resolve. Head position can also play an important role, especially when the bubble becomes too small to cover the whole cornea. In a decubitus position, the bubble is more effective for sealing off the incision site (Fig. 1G, 1H). Previous studies have also recommended considering a superior rather than temporal incision, to facilitate gas tamponade in a routine sitting up position [3]. We suggest that gas tamponade at the incision site with an appropriate position would also be effective in standard cases of DMD. Also, it may have been better if we had utilized the scleral tunnel approach rather than the clear corneal incision.
In conclusion, surgeons should be cautious when operating on apparently normal eyes in patients with a history of DMD in the fellow eye. Even in uneventful surgeries, DMD should be investigated carefully and if detected, immediate gas tamponade at the incision site is recommended, with proper head positioning for sealing off the Descemet's membrane break.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.