Distance Suppression as a Predictive Factor in Progression of Intermittent Exotropia
Article information
Abstract
Purpose
To address the natural course of intermittent exotropia with small exodeviations (less than 20 prism diopters [PD]) according to the status of suppression, and to evaluate whether suppression testing at the initial visit can assist in predicting the progression of intermittent exotropia.
Methods
Clinical records of patients at the Korea University Anam Hospital, Seoul, Korea diagnosed between January 2014 and December 2018 with basic-type intermittent exotropia and initial distance deviations of less than 20 PD, older than four years of age and a minimum of three follow-up visits within a 6-month span were retrospectively reviewed. The participants were divided into two groups, the suppression group and the non-suppression group, based on the Vectogram results at the initial visit. Clinical characteristics, rate of surgery, and rate of progression were compared between the two groups.
Results
A total of 71 patients were included. Among them, 16 patients (22.5%) had visual suppression at the initial visit, while 55 patients (77.5%) had no suppression. At the initial visit, the mean distant angle of deviation was 13.7 ± 3.2 PD (range, 4 to 18 PD) in the suppression group and 12.7 ± 3.4 PD (range, 10 to 18 PD) in the non-suppression group. Ten patients (62.5%) underwent surgery in the suppression group and 12 patients (21.8%) underwent surgery in the non-suppression group (p < 0.01). Eleven patients (68.8%) in the suppression group and 13 (23.6%) in the non-suppression group developed progression (p < 0.01).
Conclusions
Suppression testing was important to predict the progression of intermittent exotropia, in patients with exodeviation angles less than 20 PD at the initial visit.
Intermittent exotropia is the most common type of childhood strabismus. Although intermittent exotropia may become worse with time, few studies have documented the natural history of untreated intermittent exotropia thus far, and the natural course of intermittent exotropia remains unclear [123456]. Although many reports have found that deviations in intermittent exotropia generally increase over time, a few studies observed that not all exodeviations were progressive and some remained unchanged over many years of observation or improved without therapy [78]. Hiles et al. [1] observed 48 patients aged 6 to 22 years who had intermittent exotropia for an average of 11.7 years with no treatment. Among them, 65% showed improvement in their exodeviation angle. Of this group, the majority of the patients were exophoric and had deviations of less than 20 prism diopters (PD).
Surgical correction of intermittent exotropia is usually considered when there is a large angle of exodeviation, loss of fusion, or cosmetic problems [9]. Unless there is a significant deterioration of fusion, surgical intervention is not recommended in patients with angles of deviation of less than 20 to 25 PD; these indivisuals instead should be placed under close observation [10]. Also, there is a lack of consensus about predictive factors for the deterioration of intermittent exotropia with small deviation angles of less than 20 PD. Rosenbaum reported that the development of suppression in intermittent exotropia preceded a loss of distance stereoacuity. He suggested that suppression testing may be an early detection test to identify the deterioration of intermittent exotropia [11]. To the best of our knowledge, there has not been any report published addressing the natural course of intermittent exotropia based on suppression test results from the initial visit.
This study therefore aims to investigate the natural course of intermittent exotropia with deviations of less than 20 PD according to the status of suppression. Additionally, it aims to evaluate whether suppression testing at the initial visit could assist with predicting the progression of intermittent exotropia.
Materials and Methods
This study was approved by the institutional review board of Korea University Medical Center (2019AN0389). Written informed consent was waived due to the retrospective nature of the study. The principles outlined in the Declaration of Helsinki were followed in this study.
Clinical records of patients at the Korea University Anam Hospital, Seoul, Korea diagnosed between January 2014 and December 2018 with basic-type intermittent exotropia and initial distance deviations of less than 20 PD who were older than four years of age and who had a minimum of three follow-up visits within a 6-month span were retrospectively reviewed.
Patients with anisometropia, amblyopia, those who had already had one or more strabismus surgeries, those with neurological abnormalities or systemic disease, and those who underwent patching therapy during the study period were excluded.
At the time of the initial visit, all subjects underwent best-corrected visual acuity measurement, manifest refraction, ocular motor testing, and suppression testing. The angle of deviation (in PD) was determined using the prism and the near (33 cm) and distance (6 m) alternate cover tests. Suppression was measured at distance fixation using the vectographic projector test (L29; Luneau Technology, Luneau, France) [12]. Patients wore polarized three-dimensional glasses and viewed two images on one side of the vectographic slide and two other images on the other side of the vectographic chart. If a patient saw all four images and reported the names of the four images at one time, they were categorized as having no suppression. If patients could see with a single eye (either right or left eye) and reported only two images on the single side of the chart, the results were recorded as “positive” and they were interpreted as having suppression in the other eye. All measurements were performed by an experienced pediatric ophthalmologist (JHK).
The study participants were then divided into two groups, a suppression group and a non-suppression group, based on the vectogram results. Follow-up appointments were performed by the same pediatric ophthalmologist (JHK). The patients were followed at one and three months and then every 6 months thereafter.
The progression of intermittent exotropia was defined as an increase in the deviation angle of more than 10 PD at the final visit or when a patient underwent strabismus surgery [6].
Patients who underwent surgery satisfied the following criteria: a positive vectogram result during follow-up at the outpatient clinic or the display of two consecutive increases in exodeviation angle. Excluded from the group were patients who sought out alternative surgical solutions to address cosmetic needs.
Age, initial and final angles of the exodeviation, follow-up periods, rate of surgery, and rate of progression were compared between the two groups. In surgical cases, the final angle of exodeviation was defined as the angle of deviation measured at one day before the surgery.
Statistical analyses were performed using IBM SPSS Statistics ver. 24 (IBM Corp., Armonk, NY, USA). The Mann-Whitney U-test and Pearson chi-squared test were used to compare the two groups, considering a critical value of 0.05.
Results
A total of 71 patients were included in this study. Among them, 16 patients (22.5 %) had visual suppression at the initial visit, while 55 patients (77.5%) had no suppression. The mean age of the patients was 7.7 ± 2.8 years (range, 4 to 15 years) in the suppression group and 7.0 ± 2.3 years (range, 4 to 13 years) in the non-suppression group. Among the 71 patients, 41 (57.7%) were male and 30 (42.3%) were female. There were no significant differences in either age or sex between the two groups.
At the initial visit, the mean distant angle of deviation was 13.7 ± 3.2 PD (range, 4 to 18 PD) in the suppression group and 12.7 ± 3.4 PD (range, 10 to 18 PD) in the non-suppression group. Additionally, the mean near angle of deviation was 14.0 ± 4.6 PD (range, 0 to 20 PD) in the suppression group and 12.5 ± 3.7 PD (range, 0 to 18 PD) in the non-suppression group. There were no significant differences in the angles of deviation at the time of the initial visit between the two groups (Table 1).
The mean follow-up period was 18.4 ± 10.2 months (range, 6 to 36 months) in the suppression group and 19.6 ± 9.6 months (range, 6 to 36 months) in the non-suppression group (p = 0.59).
As demonstrated in Fig. 1A and 1B, the mean angle of deviation increased in both groups. When adopting an increase of the deviation angle of more than 10 PD as the standard of progression, 11 patients (68.8%) in the suppression group and 13 patients (23.6%) in the non-suppression group had progressed.
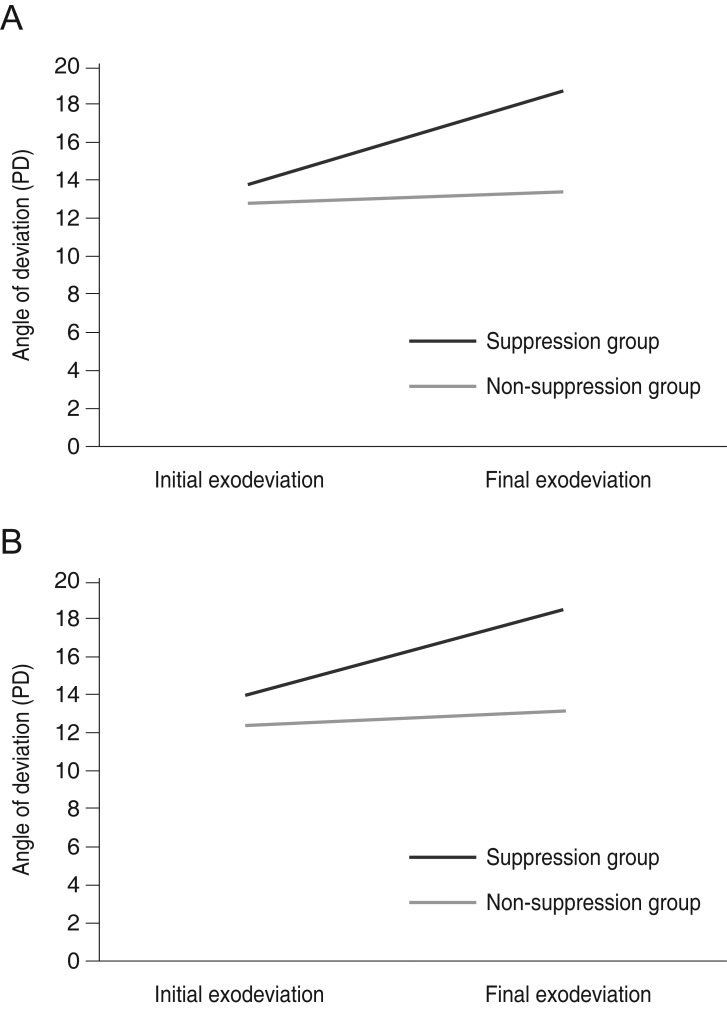
The change in the angle of deviation at initial visit and at final visit (A)Distance (B)Near PD = prism diopters.
Comparisons of clinical data at the final visit between the suppression group and the non-suppression group are summarized in Table 2. At the final visit, the mean distant angle of deviation was 18.7 ± 7.7 PD (range, 4 to 30 PD) in the suppression group and 13.4 ± 7.5 PD (range, 0 to 30 PD) in the non-suppression group (p < 0.01). Also, the mean near angle of deviation was 18.6 ± 8.3 PD (range, 0 to 30 PD) in the suppression group and 13.2 ± 7.9 PD (range, 0 to 30 PD) in the non-suppression group (p < 0.01).
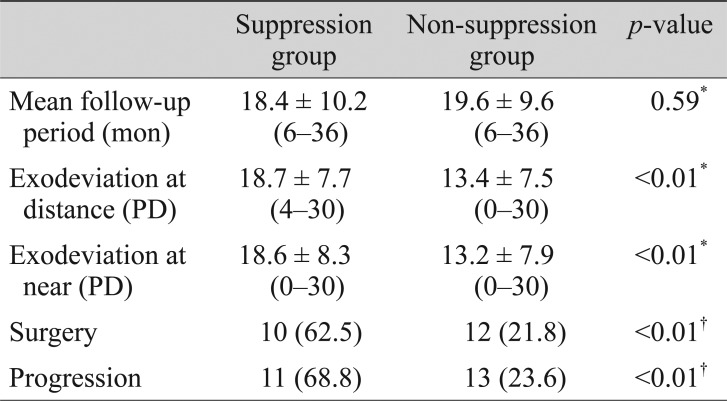
Comparison of clinical data at the final visit between the suppression group and the non-suppression group
Ten patients (62.5%) underwent surgery in the suppression group and 12 (21.8%) underwent surgery in the non-suppression group (p < 0.01), respectively, for a significantly higher incidence of surgery in the suppression group. Eleven patients (68.8%) in the suppression group and 13 (23.6%) in the non-suppression group developed progression. This difference was statistically significant (p < 0.01). Patients who showed suppression at the time of their initial visit were likely to have progressed by the final visit and to have undergone surgery during the follow-up period (Fig. 2A, 2B).
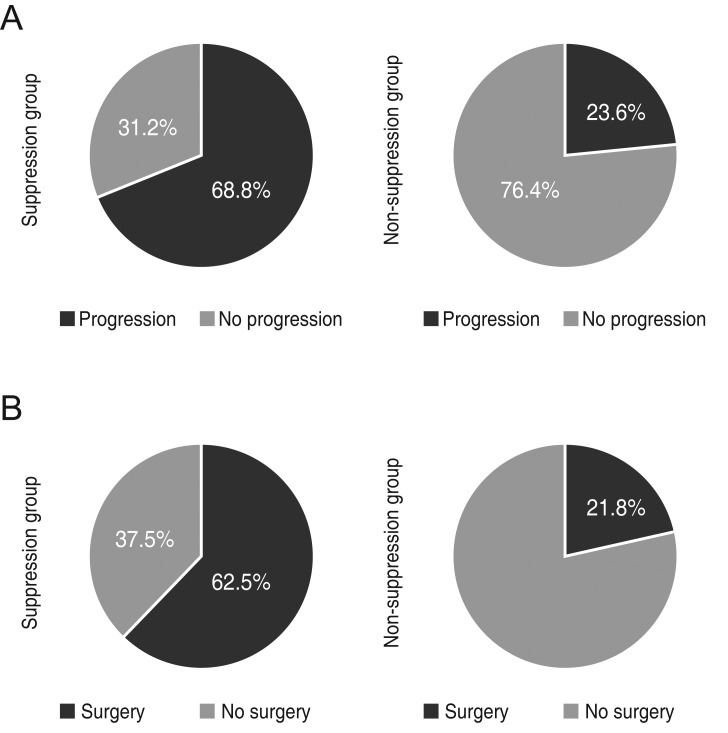
Pie graphs showing the percentage of patients partitioned by (A) progression during the follow-up period and (B) surgery during the follow-up period.
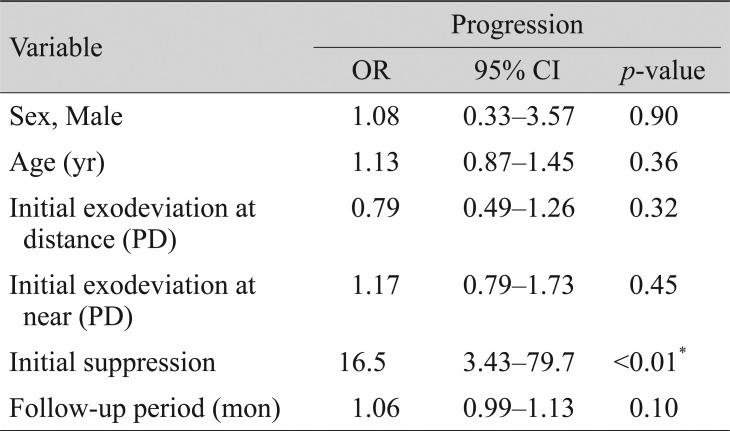
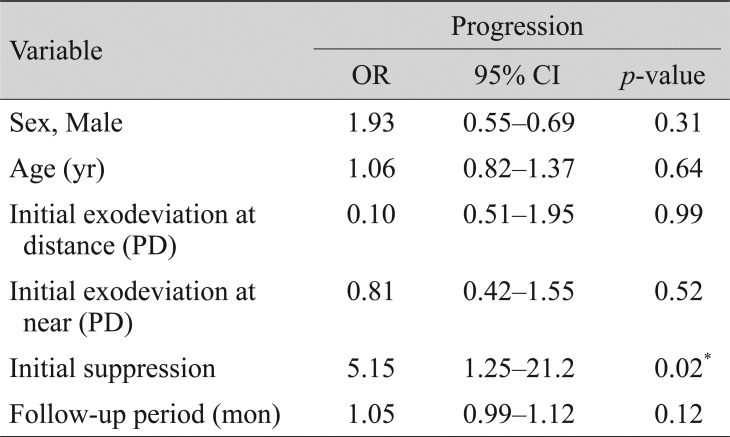
Using multivariate logistic regression analysis, the suppression identified during the initial visit was the only significant factor associated with progression (odds ratio, 16.5; 95% confidence interval, 3.43 to 79.7; p < 0.01) (Table 3), and surgery (odds ratio, 5.15; 95% confidence interval, 1.25 to 21.2; p = 0.02) (Table 4).
Discussion
This study was performed to identify whether suppression testing at the time of initial visit could predict the progression of intermittent exotropia in patients with exodeviation angles of less than 20 PD. In this study, we found that patients with suppression observed at the initial visit were likely to display progression at the final visit.
In previous studies, researchers suggested that suppression is an important prognostic factor in intermittent exotropia. Von Noorden and Campos [10] observed 51 patients aged 5 to 10 years with no treatment for an average of 3.5 years. In this group, 75% showed progression, 16% showed improvement, and 9% showed no change. Based on these results, Von Noorden and Campos [10] identified four key factors that affect progression, as follows: decreased tonic convergence with increasing age, development of suppression, loss of accommodative power, and increased divergence of orbit with advancing age. The results also suggested the possibility of that the development of suppression could have a role in the progression of intermittent exotropia. Jampolsky [13] and Jampolsky [14] postulated that exodeviations begin as a case of exophoria that may progress to intermittent exotropia, eventually becoming constant exotropia as suppression develops. He considered suppression to be the key that unlocks the fusion mechanisms.
Our results confirmed the previous suggestion that suppression at the initial visit could deteriorate intermittent exotropia. Early suppression tests were a helpful predictive factor associated with the progression of intermittent exotropia and could inform decisions regarding the timing of therapeutic interventions.
Several points need to be considered when interpreting our results. First, this study was limited by its retrospective design and the small number of cases included. Cases were not evenly distributed according to suppression, which may have influenced the results. Thus, further research with large and more evenly distributed cases may be needed to investigate the clinical usefulness of suppression testing. Second, we analyzed patients with minimum of 6-month follow-up periods, and this time period is shorter than that usually needed to determine the natural course of intermittent exotropia. Lastly, in this study, the control of intermittent exotropia was assessed using a previously described control scale for each patient [15]. All of the patients were exophoric, and rated from 0 to 2 points at their initial visit. Our study focused on initial visual suppression, but additional studies could evaluate the role of assessing control in predicting the prognosis of intermittent exotropia as well.
In conclusion, suppression testing is an important predictor of the progression of patients with intermittent exotropia with deviations of less than 20 PD at the time of their initial visit.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.