 |
 |
| Korean J Ophthalmol > Volume 32(1); 2018 > Article |
Abstract
Purpose
To evaluate changes in clinical practice in the field of refractive surgery in Korea over the past 10 years.
Methods
A survey consisting of 59 multiple-choice questions regarding the preferred types of refractive surgery, excimer laser machine, and presbyopia surgery was mailed to 742 members of the Korean Society of Cataract and Refractive Surgery in January 2016, and 50 members responded to the survey. These data were compared with the 2005 or 2007 survey results.
Results
The majority of respondents were in their 40s (54%), and the average number of refractive surgeries performed in one month was 53. The most commonly used excimer laser machine was the VISX S4 in both 2005 (32%) and 2015 (25%); however, a greater variety of machines (EX500 [18%], Allegretto wave Eye-Q [13%], AMARIS 750 [10%]) were used in 2015. The preferred corneal refractive surgery in 2015 was surface ablation (40%), representing a significant increase in its popularity compared to 2005 (15%) (p < 0.001). The popularity of laser in situ keratomileusis (LASIK) surgery decreased to 20% in 2015 compared to 48% in 2005 (p < 0.001). Eighty percent of LASIK procedures in 2015 were performed using femtosecond laser. In 2015, surface ablation and phakic intraocular lens implantation were preferred for the treatment of myopia less than -8 diopters and more than -8 diopters, respectively. The proportion of respondents performing presbyopia surgery in 2015 (76%) was significantly increased from 2007 (30%) (p < 0.001).
The first refractive surgery technique, radial keratotomy, was introduced in the 1970's. In 1988, photorefractive keratectomy (PRK) was developed by Mennerlyn; in 1990, Pallikaris developed laser in situ keratomileusis (LASIK). PRK and LASIK are still widely used clinically [1,2]. To compensate for the disadvantages of LASIK such as corneal ectasia, epithelial ingrowth, and complications related to the corneal flap, laser epithelial keratomileusis (LASEK) was developed in 1999 by Camellin [3]. Phakic intraocular lenses (IOLs) have become a promising surgical option for the treatment of high myopia, where use of the excimer laser has been hindered by night halos, glare, corneal haze, and limitation of corneal ablation depth. Refractive surgery trends are rapidly evolving. Identifying the current practices in the field of refractive surgery and comparing them with the practices of the past are important for predicting future changes in refractive surgery and eye care policy research.
We have routinely surveyed the practices of refractive surgery in Korea since 1995. In this study, we analyze the results of a 2015 survey that was provided to members of the Korean Society of Cataract and Refractive Surgery (KSCRS) regarding types of refractive surgery performed, use of the excimer laser machine, and performance of presbyopia surgery. By comparing the results of this survey to others conducted during the past 10 years, changes in the practice of refractive surgery can be elucidated.
The questionnaire analyzed in this study is based on one that was used in a previous survey, and was intended to uncover the current practices in refractive surgery [4]. The questionnaire consisted of 59 multiple-choice questions, written in accordance with the survey of the International Society of Refractive Surgery (ISRS). Questions were intended to provide information about individual surgeons, types of refractive surgery performed, use of the excimer laser, preferred refractive surgery according to diopter range, complications after refractive surgery, and performance of presbyopia surgery.
The survey was mailed to 742 members of the KSCRS in January 2016. Surveys returned before January 30, 2016, were analyzed, and the results were compared to those of 2005 and 2007 surveys. Presbyopia surgery was not included in the 2005 survey but was in the 2007 survey. Fifty members responded to this survey, resulting in a response rate of 6.7%, lower than the 18.0% response rate obtained in 2005 [4]. PASW Statistics ver. 18.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis.
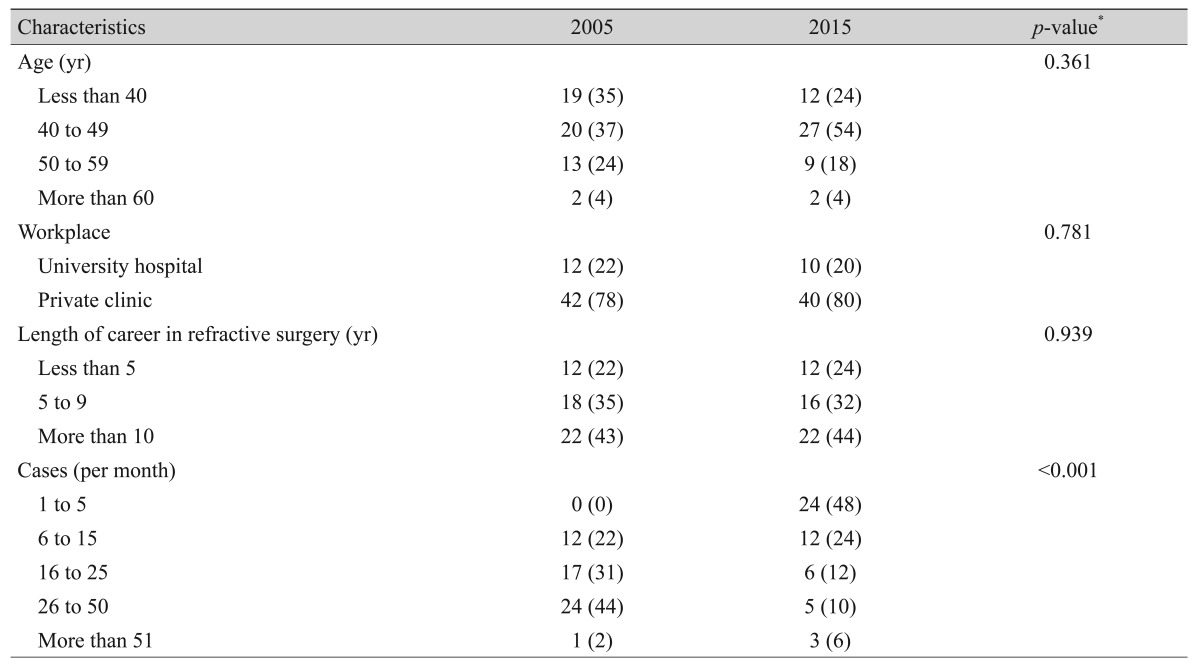
The majority of respondents (54%) were 40 to 49 years of age, 24% were less than 40 years of age, and 18% were 50 to 59 years of age. The age distribution was similar to that identified in the 2005 survey (chi-square test, p = 0.361) (Table 1). Forty-four percent of the respondents had a refractive surgery career spanning more than 10 years, while 32% had been practicing refractive surgery for 5 to 9 years. Workplace distribution was also similar to that observed in 2005 (chi-square test, p = 0.939) (Table 1). Eighty percent of the respondents worked in a private clinic, while the remainder worked in a university hospital. Forty-eight percent of the respondents performed one to five refractive surgeries a month, 24% performed 6 to 15, 12% performed 16 to 25, 10% performed 26 to 50, and 6% performed more than 51 refractive surgeries a month. These numbers were significantly lower than those reported in 2005 (44% performed 26 to 50 refractive surgeries a month, 31% performed 16 to 25, 22% performed 6 to 15, and 2% performed more than 51 refractive surgeries a month; chi-square test, p < 0.001) (Table 1).
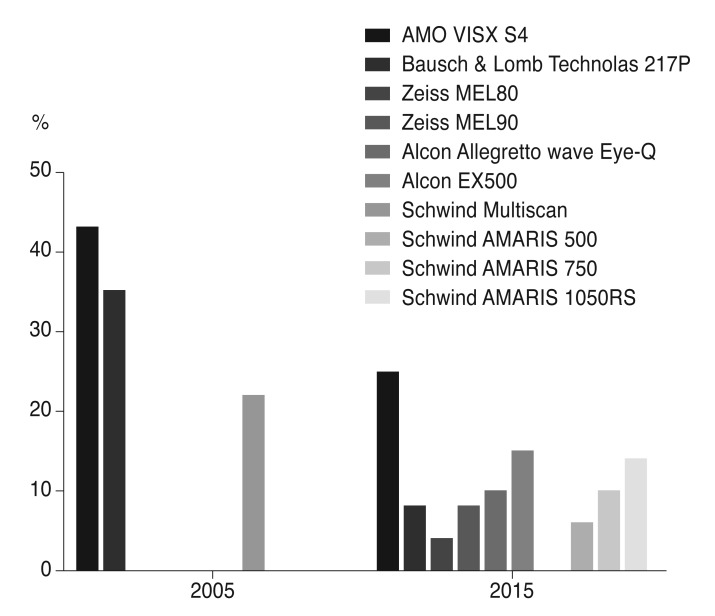
The most commonly used excimer laser machine was the VISX STAR S4 IR (AMO, Santa Ana, CA, USA) (25%). However, the proportion of surgeons using the machine had decreased since 2005 (43%) due to the availability of a larger variety of excimer laser machines. Alternatives included the EX500 (Alcon, Fort Worth, TX, USA) (15%), AMARIS 1050RS (SCHWIND, Kleinostheim, Germany) (14%), AMARIS 750 (SCHWIND) (10%), Allegretto wave Eye-Q (Alcon) (10%), Technolas 217P (Technolas Perfect Vision GmbH, Munich, Germany) (8%), and MEL 90 (Carl Zeiss Meditec AG, Jena, Germany) (8%) (Fig. 1).
Results of the 2015 survey revealed that all respondents assessed central corneal thickness, anterior chamber depth, corneal topography, corneal keratometry, fundus status, pupil size in dim light, and intraocular pressure as part of their preoperative examination. Eighty-six percent of respondents performed a Schirmer's test or assessed tear film break-up time, 80% performed infrared pupillometry, 77% performed an endothelial cell count, 67% used a wavefront analyzer, 68% measured axial length, and 68% measured peripheral corneal thickness.
The most commonly performed refractive surgery in 2015 was surface ablation. Its popularity increased from 15% of all refractive surgeries performed in 2005 to 40% in 2015. On the other hand, LASIK, which comprised 81% of all refractive surgeries performed in 2005, decreased significantly to only 35% in 2015 (chi-square test, p < 0.001) (Fig. 2). In 2015, the popularity of phakic IOL implantation increased significantly from 4% in 2005 to 21% (chi-square test, p < 0.001) (Fig. 2). Small incision lenticule extraction LASIK comprised 4% of the refractive surgeries performed in 2015. We found that the preferred surgery changed according to the spherical equivalent. In 2005, LASIK was the preferred surgery for measurements of less than -4 diopters (D) (87%) as well as measurements of -4 to -8 D (81%). However, in 2015, surface ablation was the preferred surgery for measurements less than -4 D (71%) as well as measurements of -4 to -8 D (71%). Regarding measurements of -8 to -12 D, LASIK (57%) was the preferred surgery in 2005, followed by phakic IOL implantation (17%). In 2015, phakic IOL implantation (58%) was the preferred surgery for this measurement range, followed by surface ablation (38%). For measurements greater than -12 D, phakic IOL implantation was the preferred surgery in both 2005 (67%) and 2015 (92%) (Fig. 3A-3D). The preferred residual stromal bed thickness limitation for LASIK in 2015 was 300 to 350 µm (66.7%), followed by 350 to 400 µm (23.1%), 250 to 300 µm (7.7%), and greater than 400 µm (2.6%) in 2015.
In 2015, the preferred corneal flap diameter was 8.5 mm (52.5%) in cases with myopia and 9.0 mm (64.0%) in cases with hyperopia. This was similar to the findings in 2005: 8.5 mm (61%) was preferred in cases with myopia, 9.0 mm (35%) was preferred in cases with hyperopia. The preferred corneal flap thickness in 2015 was 130 µm (66%), followed by less than 120 µm (31%). This was slightly different from the findings of the 2005 survey (130 µm [76%], 160 µm [20%]) (chi-square test, p < 0.001). Sixty-seven percent of respondents in 2015 used a wavefront analyzer; this was similar to the percentage using preoperative wavefront analysis in 2005 (76%) (chi-square test, p = 0.210). The percentage of ‘yes’ answers to the question asking whether the use of preoperative wavefront analysis resulted in better surgical results decreased from 57% in 2005 to 36% in 2015 (chi-square test, p < 0.001) (Fig. 4A, 4B). The preferred refractive surgery in 2015 was surface ablation (46%), while it had been LASIK (48%) in 2005 (chi-square test, p < 0.001).
Of the LASIK procedures performed in 2015, 80% were conducted using femtosecond laser. Frequently used femtosecond laser machines were IntraLase Femtosecond laser (AMO) (52%), VisuMax (Cal Zeiss Meditec) (24%), LDV Z4 (Ziemer, Port, Switzerland) (17%), and LDV Cristal line (Ziemer) (7%). Forty-six percent of respondents used mitomycin-C for every surface ablation, and 54% used it on a case by case basis. The preferred methods of phakic IOL were posterior chamber phakic IOL (ICL; STAAR Surgical, Nidau, Switzerland) (74%), Artif lex iris-claw phakic IOL (Ophtec BV, Groningen, the Netherlands) (16%), and Artisan iris-claw phakic IOL (Ophtec BV) (10%).
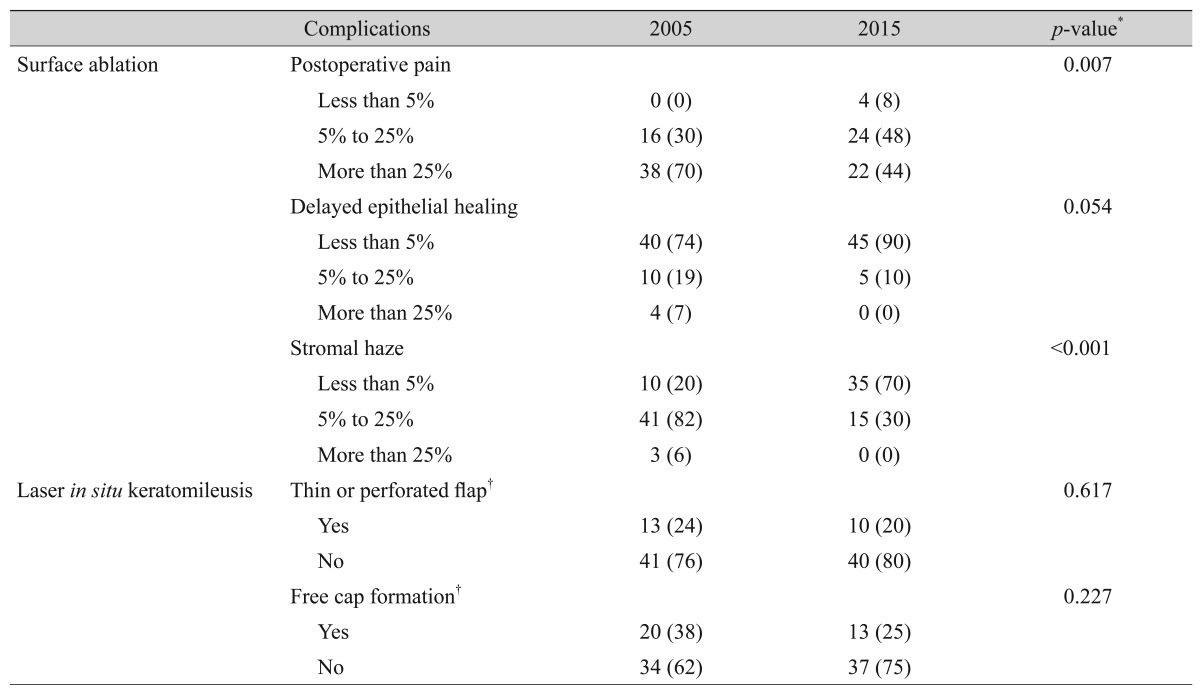
The most common complications following surface ablation were postoperative pain, delayed corneal epithelial healing, and stromal haze. Major complications of LASIK included free cap formation and thin or perforated flap. Chronic postoperative pain and delayed epithelial healing were defined as those lasting more than three days after surgery. Seventy percent of respondents in 2005 reported pain in more than 25% of patients, while 48% of respondents in 2015 reported pain in only 5% to 25% of patients. Seventy-six percent of respondents in 2005 identified stromal haze in 5% to 25% of patients [4], while 70% of respondents in 2015 identified stromal haze in less than 5% of patients (Table 2). Percentage of respondents who encountered a free flap during surgery decreased from 38% in 2005 to 25% in 2015 (thin or perforated flap, p = 0.617; free flap, p = 0.227) (Table 2).
The percentage of respondents performing presbyopia surgery increased significantly from 30% in 2005 to 75% in 2015 (chi-square test, p < 0.001). In 2015, 58%, 25%, and 17% of respondents performed presbyopia surgery for both hyperopia and myopia, only myopia, and only hyperopia, respectively. Types of surgery included lens extraction with multifocal IOL implantation (45%), excimer laser (42%), and corneal inlay (13%). AcrySof ReSTOR (Alcon) (31.5%), Tecnis ZM900 (AMO) (26.5%), Lentis Mplus (Oculentis, Berlin, Germany) (20.5%), and AT LISA 839MP (Carl Zeiss) (15%) were the most frequently used IOLs for presbyopia correction in 2015. The proportion of respondents performing a monovision technique with a monofocal IOL was 6.5%. Raindrop Near Vision Inlay (ReVision Optics, Lake Forest, CA, USA)was preferred by 92% of the respondents who performed corneal inlay. The percentage of cases requiring additional correction with the excimer laser for postoperative refractive error after IOL implantation was 76%. Additional correction was mainly accomplished with surface ablation (77%). Satisfaction ratings for presbyopia surgery differed according to the procedure performed. Ninety-seven percent of surgeons responded that their patients were satisf ied with lens extraction with IOL implantation, while only 50% responded that their patients were satisfied with corneal inlay. Complaints included ‘blurred vision at long distance’ (30%), ‘halo and glare’ (21%), ‘blurred vision at all distances’ (20%), and ‘eye dryness’ (18%).
This study investigated the current trends in refractive surgery, as well as the changes occurring between 2005 and 2015. The survey used in this study had a similar format t o t hose r outinely administered t o t he m embers of KSCRS since 1995. Over the past 10 years, the preferred corneal refractive surgery changed from LASIK to surface ablation, and the popularity of phakic IOL implantation and presbyopia surgery has markedly increased.
In both the 2005 and 2007 surveys, LASIK was the most commonly performed refractive surgery and was preferred in cases with myopia of less than -8 D as well as measurements from -8 to -12 D [4,5,6]. However, surface ablation was preferred in cases with myopia of less than -8 D, and phakic IOL implantation was preferred in cases with myopia greater than -8 D. This study revealed a decreased incidence of postoperative pain and corneal haze following surface ablation over the past 10 years. This might be due to development of the excimer laser machine and appropriate preoperative pain control such as with topical nonsteroidal anti-inflammatory drugs [7,8]. On the contrary, the incidence of critical flap-related complications with LASIK was similar between 2005 and 2015. This might be the reason for the greater popularity of surface ablation than LASIK. In a 2015 survey conducted by ISRS, LASIK was performed most often in cases with myopia of less than -8 D (56%), while phakic IOL implantation was preferred in cases with myopia of greater than -8 D (33%) [9]. Because the central cornea is relatively thin in Koreans as compared to westerners, and because greater corneal ablation depth is needed due to the higher degree of myopia in Asian people versus Americans and Hispanics, the popularity of surface ablation in Korea might be higher than in the USA [10,11]. Another possible explanation is that Korean surgeons might avoid LASIK because of the possibility of flap-related complications, which are difficult to treat. In cases with high myopia, phakic IOL implantation might be a better alternative, reducing the incidence of complications such as corneal ectasia, postoperative refractive error, and myopic regression. However, meticulous attention is needed to avoid such complications as cataract formation, elevated intraocular pressure, and loss of corneal endothelium [12,13,14,15]. Respondent characteristics including age and surgical experience in the 2015 survey were similar to those in the 2005 survey; however, the average number of refractive surgeries performed monthly radically decreased over the past 10 years. This could be the result of the continuing economic recession and competition among university hospitals and private ophthalmology clinics. Regarding the excimer laser machine, in 2015, up to 94% of US clinicians used the VISX (AMO) and wavelight (Alcon), while Korean clinicians used a greater variety of machines [9]. In Korea, the preferred minimum residual stromal bed thickness for LASIK was 300 to 350 µm (66.7%), followed by 350 to 400 µm (23.1%). In comparison, the preferred residual stromal bed thicknesses were 300 µm (43%), 250 µm (39%), and 275 µm (16%) in the USA. Korean surgeons, indicating a preference for thicker residual stromal beds. This could be related to the Korean surgeon's tendency to avoid corneal ectasia related to refractive surgery and to prepare for additional surgery with a residual stromal bed. The preferred thickness of the corneal flap was 130 µm in both 2005 and 2015, with some respondents liking a thinner flap. This might be because a thin flap can be created more easily using a femtosecond laser. The frequency of wavefront analyzer use in 2015 was similar to that in 2005; however, belief about association between preoperative wavefront analyses and better surgical results was reduced. It is thought that the development of excimer laser machines results in good surgical outcomes regardless of the use of preoperative wavefront analysis.
As the population ages and the elderly remain economically active, there has been rapid increase in the need for presbyopia surgery over the past 10 years. The majority of presbyopia surgeries detailed in this survey were multifocal IOL implantation and excimer laser surgeries. Patient satisfaction with multifocal IOL implantation was high (97%) in this study; however, we think that this result seems to be slightly different from other studies [16,17]. The 2015 survey conducted by ISRS revealed a 70% preference for monovision or modified monovision with monofocal IOL surgery. This finding was markedly different from that revealed by the Korean survey. Perhaps this is due to differences between US medical insurance (Medicare and Medicaid) and the national health insurance of Korea. Significantly less satisfaction with corneal inlay (50%) was noted in this study compared to published reviews [18,19]. Further research is required regarding presbyopia surgery. Presbyopia surgery is a promising field, and we think that upcoming results will demonstrate increasing excellence.
This study had several limitations. First, this survey was comprised of multiple-choice questions; therefore, selection bias could be induced if the respondent's desired answer was not available. Second, the response rate was limited because this was anonymous survey. Third, opinions of ophthalmologists who are not KSCRS members were not included.
In conclusion, the preferred refractive surgery has changed from LASIK to surface ablation, and the popularity of presbyopia surgery has increased significantly over the past decade. Finally, thank you to all KSCRS members who have taken the time to respond to these surveys, a total of 14 in 21 years. We hope for your continued participation in future surveys.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Munnerlyn CR, Koons SJ, Marshall J. Photorefractive keratectomy: a technique for laser refractive surgery. J Cataract Refract Surg 1988;14:46-52.


2. Pallikaris IG, Papatzanaki ME, Siganos DS, Tsilimbaris MK. A corneal flap technique for laser in situ keratomileusis. Human studies. Arch Ophthalmol 1991;109:1699-1702.


5. Ku M, Shyn KH. 2006 Survey for KSCRS members: current trends in refractive surgery in Korea. J Korean Ophthalmol Soc 2009;50:182-188.

6. Paik HJ, Song HJ, Shyn KH. 2007 Survey for K SCRS members: current trends in cataract surgery in Korea. J Korean Ophthalmol Soc 2009;50:1624-1631.

7. Hong JP, Nam SM, Im CY, et al. Comparison of analgesic effect of preoperative topical diclofenac and ketorolac on postoperative pain after photorefractive keratectomy. J Cataract Refract Surg 2014;40:1689-1696.


8. Hansen RS, Lyhne N, Grauslund J, et al. Four-year to seven-year outcomes of advanced surface ablation with excimer laser for high myopia. Graefes Arch Clin Exp Ophthalmol 2015;253:1027-1033.


9. Duffey RJ, Leaming D. US trends in refractive surgery: 2015 ISRS survey [Internet]. Las Vegas: American Academy of Ophthalmology; 2015. cited 2017 Nov 30. Available from: http://isrs.aao.org/Assets/61d6958b-696a-4888-b539-757156c28663/635839820892400000/2015-us-trends-survey-presentation-pdf.
10. Hwang YH, Kim HK, Sohn YH, e t. C entral c orneal thickness in a Korean population: the Namil Study. Invest Ophthalmol Vis Sci 2012;53:6851-6855.


11. Brandt JD, Beiser JA, Kass MA, Gordon MO. Central corneal thickness in the Ocular Hypertension Treatment Study (OHTS). Ophthalmology 2001;108:1779-1788.


12. Goker S, Er H, Kahvecioglu C. Laser in situ keratomileusis to correct hyperopia from +4.25 to +8.00 diopters. J Refract Surg 1998;14:26-30.


13. Geggel HS, Talley AR. Delayed onset keratectasia following laser in situ keratomileusis. J Cataract Refract Surg 1999;25:582-586.


14. Lyle WA, Jin GJ. Laser in situ keratomileusis with the VISX Star laser for myopia over -10.0 diopters. J Cataract Refract Surg 2001;27:1812-1822.


15. Fernandes P, Gonzalez-Meijome JM, Madrid-Costa D, et al. Implantable collamer posterior chamber intraocular lenses: a review of potential complications. J Refract Surg 2011;27:765-776.


16. Schmickler S, Bautista CP, Goes F, et al. Clinical evaluation of a multifocal aspheric diffractive intraocular lens. Br J Ophthalmol 2013;97:1560-1564.


17. Mendicute J, Kapp A, Levy P, et al. Evaluation of visual outcomes and patient satisfaction after implantation of a diffractive trifocal intraocular lens. J Cataract Refract Surg 2016;42:203-210.


Fig. 2
Preferred refractive surgeries in 2005 and 2015. LASIK = laser in situ keratomileusis; IOL = intraocular lens; SMILE = small incision lenticule extraction.
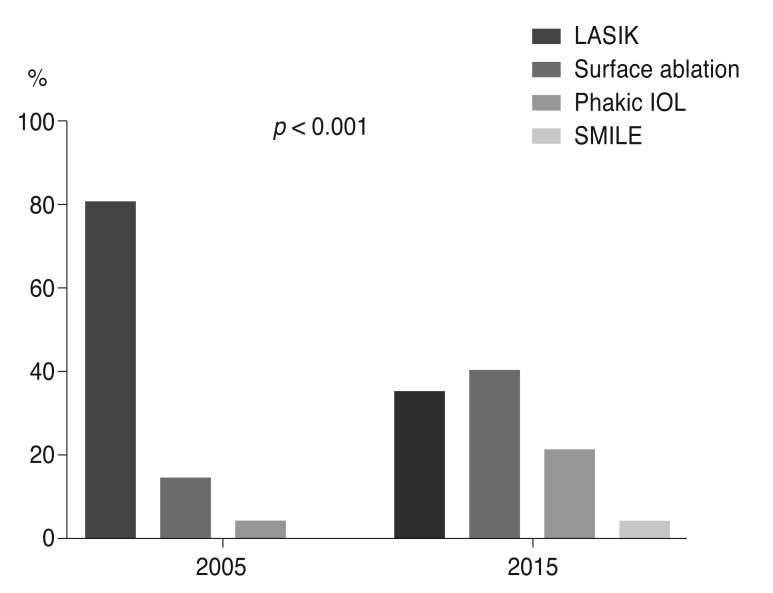
Fig. 3
Preferred refractive surgeries according to spherical equivalent in 2005 and 2015 (A) less than -4 diopters (D), (B) -4 to -8 D, (C) -8 to -12 D, (D) more than-12 D. LASIK = laser in situ keratomileusis; IOL = intraocular lens; SMILE = small incision lenticule extraction; CLE = clear lens extraction.

Fig. 4
Changes in respondents' perceptions regarding preoperative wavefront analysis in refractive surgery between 2005 and 2015. (A) Whether or not to perform wavefront analysis before refractive surgery. (B) Whether or not preoperative wavefront analysis results in better outcomes following refractive surgery.




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




