Bilateral Arteritic Anterior Ischemic Optic Neuropathy Associated with Giant Cell Arteritis in Korea
Article information
Dear Editor,
Arteritic anterior ischemic optic neuropathy (AAION) is caused by vascular occlusion of the posterior ciliary arteries that supply the optic nerve head (ONH). AAION is the most common ophthalmic complication associated with giant cell arteritis (GCA), and can cause sudden and permanent visual loss. It is recommended that high-dose steroid therapy should be started immediately to prevent permanent visual loss [1]. There have been few reports of AAION affecting Asians [234]. One case of AAION associated with GCA, which was confirmed by temporal artery biopsy and exhibited typical systemic symptoms, was reported by our research team in Korea [5]. Here we report a case of bilateral AAION associated with GCA in an elderly Korean man, as confirmed by temporal artery biopsy.
An 82-year-old man presented to our hospital for evaluation two days after suffering sudden vision loss in both eyes. He had a history of hypertension, chronic kidney disease, and dilated cardiomyopathy. He had also been suffering from bilateral jaw claudication for one month. His visual acuity was finger count in the right eye and hand movement in the left eye, with intraocular pressure measurements of 12 and 14 mmHg, respectively. There was no pain with eye movement. Funduscopic examination revealed a chalky white swelling of the ONH in both eyes, as well as focal retinal edema adjacent to the ONH in the right eye due to the occlusion of the cilioretinal artery (Fig. 1A). Fluorescein angiography revealed delayed filling of the optic disc and adjacent choroid in both eyes. The patient's body temperature was normal, but the C-reactive protein level, and the erythrocyte sedimentation rate were elevated to 3.04 mg/dL (upper limit of normal, 0.3 mg/dL) and 58 mm/hr (upper limit of normal, 20 mm/hr), respectively. The patient was admitted to the hospital with a presumptive diagnosis of AAION with GCA and was started on intravenous corticosteroid therapy (1 g/day for 3 days). In addition, ultrasonography and biopsy of the temporal artery as well as brain magnetic resonance imaging were planned to definitively diagnosis GCA and to differentiate it from carotid artery disease.
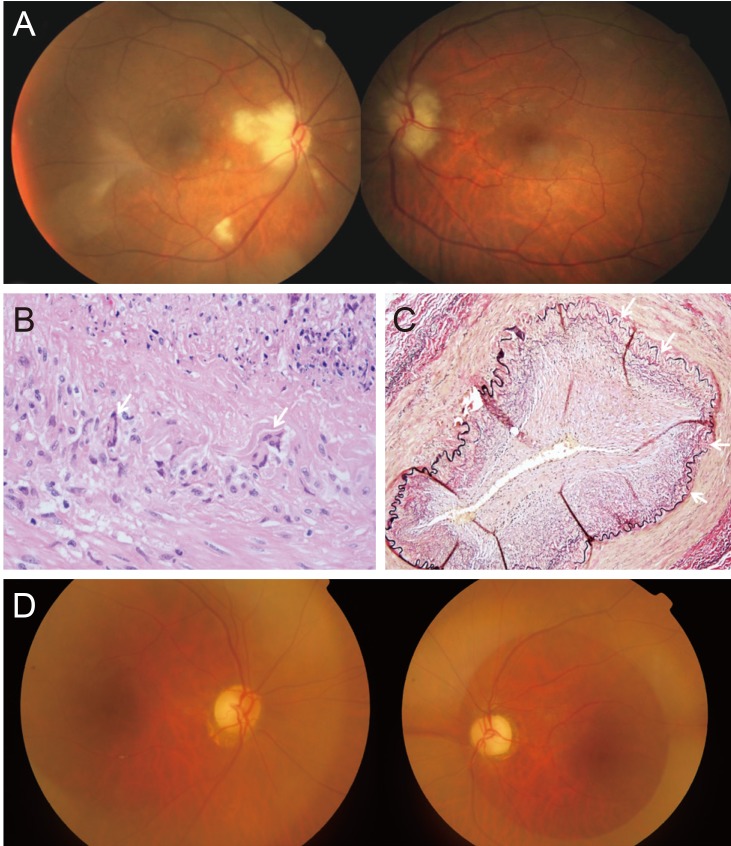
(A) Fundus photographs obtained during initial examination shows chalky, white swelling of both optic nerve heads and a focal retinal edema adjacent to the right optic nerve heads secondary to occlusion of the cilioretinal artery. (B,C) Histopathology examination of a right temporal arterial biopsy sample. (B) Multiple granulomas and giant cells in the vessel wall (H&E stain, ×100). (C) Diffuse vasculitis and interrupted elastic lamina fibers in the arterial wall (elastin stain, ×40). (D) After 3 months of treatment, a pale optic disc was visualized in both eyes.
On day two of hospitalization, temporal artery ultrasonography revealed no evidence of temporal arteritis. A biopsy of both temporal arteries was performed. Staining with hematoxylin and eosin revealed diffuse vasculitis with multiple granulomas and giant cells within the arterial walls (Fig. 1B). Elastin staining revealed discontinuous elastic fibers (Fig. 1C). A diagnosis of GCA was thereby confirmed and therapy with intravenous steroids was continued. Brain magnetic resonance imaging revealed mild stenosis of the distal aspect of the internal carotid arteries as well as of the proximal segment of the left middle cerebral artery.
On day four of hospitalization, jaw claudication was slightly improved and C-reactive protein and erythrocyte sedimentation rate levels had decreased to 0.32 mg/dL and 16 mm/hr, respectively. However, the patient's visual acuity was unchanged, and the chalky white swelling of the ONH persisted in both eyes. Oral prednisolone therapy was continued at 80 mg per day. After 10 days, the patient was transferred to another hospital of his own accord.
After three months, the patient's visual acuity remained at finger count in the right eye and hand movement in the left eye. In addition, funduscopic examination revealed a pale ONH fundus in both eyes (Fig. 1D). Optical coherence tomography demonstrated decreased thickness of the macular ganglion cell layer and the retinal nerve fiber layer in both eyes. Oral prednisolone therapy was maintained at 30 mg combined with methotrexate at 10 mg by the rheumatologic department.
Here we present a case of bilateral AAION with histologically proven GCA and typical systemic symptoms in an elderly Korean man. Previous reports described only unilateral AAION associated with GCA in Koreans [25]. To the best of our knowledge, this is the first report of a biopsy-confirmed case of bilateral AAION associated with GCA.
In conclusion, although GCA-associated AAION is rare in Korea, the incidence rate has recently increased. This report suggests that elderly patients with sudden vision loss, systemic symptoms like jaw claudication, and corresponding laboratory findings should be evaluated for GCA and treated immediately with intravenous steroids when AAION associated with GCA is suspected.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.