 |
 |
| Korean J Ophthalmol > Volume 31(5); 2017 > Article |
Abstract
Purpose
In the present study, the visual discomfort induced by smart mobile devices was assessed in normal and healthy adults.
Methods
Fifty-nine volunteers (age, 38.16 ± 10.23 years; male : female = 19 : 40) were exposed to tablet computer screen stimuli (iPad Air, Apple Inc.) for 1 hour. Participants watched a movie or played a computer game on the tablet computer. Visual fatigue and discomfort were assessed using an asthenopia questionnaire, tear film break-up time, and total ocular wavefront aberration before and after viewing smart mobile devices.
Results
Based on the questionnaire, viewing smart mobile devices for 1 hour significantly increased mean total asthenopia score from 19.59 ± 8.58 to 22.68 ± 9.39 (p < 0.001). Specifically, the scores for five items (tired eyes, sore/aching eyes, irritated eyes, watery eyes, and hot/burning eye) were significantly increased by viewing smart mobile devices. Tear film break-up time significantly decreased from 5.09 ± 1.52 seconds to 4.63 ± 1.34 seconds (p = 0.003). However, total ocular wavefront aberration was unchanged.
Smart mobile devices have increased in popularity among the general population; they have many benefits in daily life, such as facilitating communication, acting as portable all-in-one devices that include a phone, camera, GPS (global positioning system), and MP3 player and assisting handicapped people by providing verbal or motion-activated applications. However, with the recent widespread use of smart mobile devices, serious psychophysical health problems have increased worldwide. In a recent report, approximately 14% of middle school students were at high risk of smartphone addiction [1]. In another report, 45% of smartphone users felt anxiety when not holding their smartphones [2]. In addition, excessive use of smart mobile devices can cause physical problems, such as neck stiffness, blurred vision, dry eyes, and wrist or back pain [3,4]. In particular, asthenopia induced by excessive viewing of computer screens (including those on smart mobile devices) is defined as computer vision syndrome (CVS) [5,6,7,8], which presents with visual, ocular and musculoskeletal (especially neck and shoulder) symptoms.
The resolution of smart mobile devices is rapidly improving. Recently, a new retina display was introduced by Apple Inc. (Cupertino, CA, USA) with a higher pixel density (iPad Air, screen size of 9.7 inches and resolution of 2,048 × 1,536 pixels) rendering text and images extremely crisp; thus, pixels are invisible to the naked eye. High-resolution displays may have an advantage because they present brighter and clearer images; however, their effect on visual fatigue is not well known.
In this study, the visual discomfort induced by smart mobile devices equipped with state-of-the-art display technology was assessed in normal, healthy adults by measuring tear film break-up time (TBUT), total ocular wavefront aberration, and visual fatigue using a questionnaire.
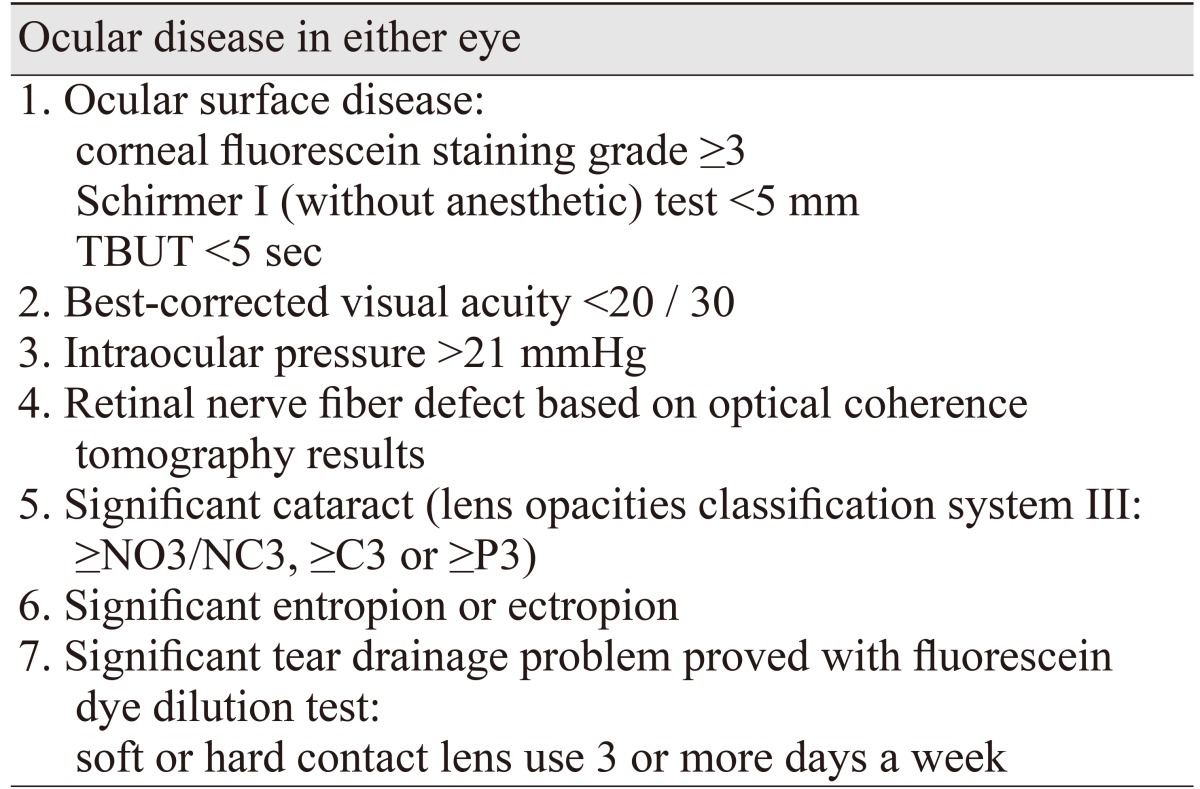
This was a prospective interventional case series study. The study followed the tenets of the Declaration of Helsinki and was approved by the institutional review board of Dongguk University Ilsan Hospital, Goyang, Korea. The purpose and design of the study were explained to all participants individually and informed consent was obtained before starting the screening test. Sixty-two healthy volunteers were recruited. Healthy subjects aged 20 to 65 years who viewed a smartphone or computer, including tablet and television, for at least 2 hours daily were included in the study. The exclusion criteria are listed in Table 1. After passing the screening test (two subjects were excluded as screening failures), 60 subjects were selected for the study; finally, 59 subjects were exposed to tablet computer screen stimuli (one subject did not show up after passing the screening).
Ophthalmic screening for participants included slit lamp microscopy, non-contact intraocular pressure measurement, fundus photography, optical coherence tomography, corrected distance visual acuity, Schirmer's I test, and TBUT.
Participants were asked to watch a tablet computer screen (iPad Air, Apple Inc.) for 1 hour at a viewing distance of approximately 40 cm. Participants watched a movie or played a computer game on the tablet computer. We allowed subjects with presbyopia the use of their reading glasses or prescribed reading glasses that felt comfortable at 40 cm. Tablet computer screen viewing was performed in the same room throughout the study period with humidity, temperature, and illumination consistently maintained; the humidity and temperature were checked every study day.
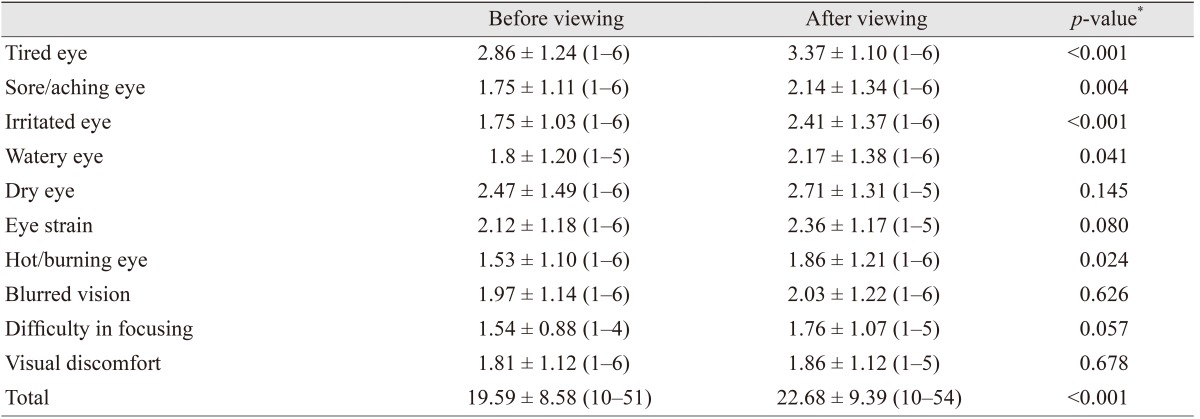
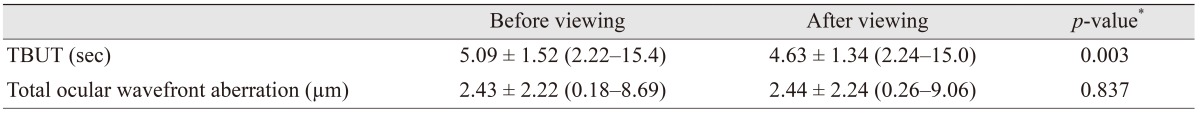
Asthenopia was evaluated using a modified version of the questionnaire developed by Ames et al. (Table 2) [9]. The questionnaire consisted of 10 questions related to asthenopia graded on a scale from 0 to 6, with 0 defined as none and 6 as most severe; a score of 60 corresponded to the most severe asthenopia. All subjects completed the questionnaire before and immediately after tablet computer use. The severity of asthenopia may change depending on daily bodily conditions, including diurnal variations and environmental factors such as illumination, humidity, and room temperature [10,11]. Therefore, to compare the effects of tablet computer watching, the asthenopia scores before and immediately after tablet computer watching (induced asthenopia) were calculated. Dysfunction of the ocular surface lubrication system induced by severe asthenopia can manifest as objective signs such as abnormal tear film and visual function. TBUT is the most commonly used clinical indicator of tear film instability, and ocular wavefront aberration can represent the precise focusing ability of the optical system. TBUT and total ocular wavefront aberration (Wavescan; VISX/Advanced Medical Optics, Santa Clara, CA, USA) were measured in the right eye of every subject before and after tablet computer viewing. The measurements were performed in triplicate and mean values were used for analysis.
Statistical analyses were performed using SAS ver. 9.3 (SAS Institute, Cary, NC, USA). Normality of data was assessed using the Shapiro-Wilk test. Changes in measured values were compared using paired t-tests and p-values less than 0.05 were considered statistically significant.
Nineteen male and 40 female participants (a total of 59 participants) were included in this study. The mean age of the participants was 38.16 ± 10.23 years (range, 22 to 64 years).
The baseline asthenopia score was 19.59 ± 8.58 and ranged from 10 to 51 (maximum possible total asthenopia score was 60), showing the study population suffered from mild to moderate asthenopia at baseline. Tired eyes, dry eyes and eye strain mean scores were above 2.0. After 1 hour of tablet viewing, the scores for five items (tired eye, sore/aching eye, irritated eye, watery eye, and hot/burning eye) were significantly increased and the mean total asthenopia score increased to 22.68 ± 9.39 (p < 0.001) (Table 3).
TBUT before tablet watching was 5.09 ± 1.52 seconds. Although the study population was chosen after strict application of exclusion criteria, the measured baseline TBUT was below the normal standard value of 10 seconds. Tablet watching induced a significant decrease of TBUT to 4.63 ± 1.34 seconds (p = 0.003). However, total ocular wavefront aberration was unchanged by tablet watching (Table 4).
In the present study, tablet computer screen watching was shown to significantly affect subjective asthenopia symptoms as well as objective TBUT. Notably, asthenopia aggravation occurred even when using state-of-the-art, high pixel density technology (improved retina display).
Smart mobile devices have become a must-have in modern life. With the widespread use of smart mobile devices, smart device addiction has become a serious health problem worldwide [12,13]. One study found that 64% to 90% of computer users develop CVS [5]. Using a computer for more than 4 hours at a time can significantly increase eye discomfort [14]. Similarly, readers of electronic books with liquid crystal display (LCD) monitors also experienced marked visual fatigue [15]. In addition, dry eye syndrome is more common in those who work on computers and has been reported in up to 60% of individuals who work with video monitors [16]. This prevalence is very high when considering the prevalence of dry eye syndrome in the general population is approximately 10% [17]. Although the exact mechanism of CVS is unclear, a decreased blink rate and increased accommodative effort are considered two possible underlying causes. Focusing on a smart mobile device screen may entail continuous accommodation effort without blinking for an extended period. One report found the blink rate during computer work significantly decreased and was negatively correlated with eye discomfort score [18]. Another study demonstrated the preferred distance for viewing a mobile device (36.2 cm) was shorter than the typical distance for reading books (40 cm) and the shorter distance required more accommodation and convergence [19]. Increased tear evaporation with decreased blinking and enhanced accommodative effort might cause dry eye aggravation with increased ocular irritation and pain, as demonstrated in the present study.
Another possible mechanism of CVS is the blue light emitted from a light emitting diode (LED) display. Although the light from an LED appears white, the wavelength of peak emission from LEDs ranges from 400 to 490 nm, in the blue light range [20]. Recently, significant concerns have been raised regarding the hazardous effects of blue light range which can damage both the cornea and the retina by inducing phototoxicity and oxidative stress [21,22,23]. A previous report found the blue light emitted from the screen of a smart mobile device can cause eye fatigue [24,20]. In addition, blocking blue light with a special lens significantly reduced visual fatigue as measured by critical flicker frequency [25]. Therefore, strategies to reduce blue light from tablet displays can be an alternative method for reducing CVS.
The duration of smart mobile device use has already reached dangerously high levels in the younger generation [26]. Prolonged daily exposure to smart mobile devices (more than 2 hours per day) is a significant risk factor for inducing multiple types of ocular discomfort [27]. However, the long-term visual effects of intense and chronic smart mobile device use have not been extensively investigated. The possible ocular health issues caused by intense smart mobile device use may not be confined to ocular surface problems such as dry eyes and tear dysfunction, but may also affect the neuronal networks of the retina.
One limitation of this study was the evaluation of visual fatigue using a questionnaire. Although the responses to questionnaires are somewhat subjective and can be affected by responders' daily physical and mental conditions, questionnaires are commonly used for assessing CVS [9,11,27]. Using an objective measurement of asthenopia would be a better alternative. However, to the best of our knowledge, no established objective method for quantifying asthenopia exists, although TBUT and wavefront analysis were used as objective methods in our study. Another limitation was the lack of a control group in this study. As mentioned earlier, many factors can cause asthenopia, however, in addition to working at close distance, using smart mobile devices alone can cause dry eye syndrome with asthenopia. Using smart mobile devices is a risk factor for dry eye because it affects blink rate and the meibomian gland [28,29,30]. In this study, there was an obvious change in the TBUT and the questionnaire before and after the work. This suggested a possibility of asthenopia due to dry eye caused by using smart devices. Because 3-dimensional images, movies and computer games provide a different stimuli to the fusion system [31], different degrees of asthenopia can occur depending on visual content. In the present study, we evaluated asthenopia only immediately after using smart mobile devices. Further research is needed to evaluate the effect of stimuli duration and degree of asthenopia dependent on visual content.
In conclusion, the results from the present study showed visual fatigue was significantly aggravated when subjects viewed a tablet computer screen for 1 hour, even though it was equipped with state-of-the-art display technology. Considering the increasing exposure to computer displays in daily life, more guidelines and investigative efforts are needed to maintain visual health.
Acknowledgements
This study was partially supported by a grant from the Korean Health Technology R&D Project through the Korean Health Industry Development Institute, funded by the Ministry of Health & Welfare, Republic of Korea (No. HI-15C1653).
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Lee H, Seo MJ, Choi TY. The effect of home-based daily journal writing in Korean adolescents with smartphone addiction. J Korean Med Sci 2016;31:764-769.



2. Choi SW, Kim DJ, Choi JS, et al. Comparison of risk and protective factors associated with smartphone addiction and Internet addiction. J Behav Addict 2015;4:308-314.



3. Kwon M, Kim DJ, Cho H, Yang S. The smartphone addiction scale: development and validation of a short version for adolescents. PLoS One 2013;8:e83558.



4. Moon JH, Lee MY, Moon NJ. Association between video display terminal use and dry eye disease in school children. J Pediatr Ophthalmol Strabismus 2014;51:87-92.


6. Rosenfield M. Computer vision syndrome: a review of ocular causes and potential treatments. Ophthalmic Physiol Opt 2011;31:502-515.


7. Blehm C, Vishnu S, Khattak A, et al. Computer vision syndrome: a review. Surv Ophthalmol 2005;50:253-262.


8. Klamm J, Tarnow KG. Computer vision syndrome: a review of literature. Medsurg Nurs 2015;24:89-93.

9. Ames SL, Wolffsohn JS, McBrien NA. The development of a symptom questionnaire for assessing virtual reality viewing using a head-mounted display. Optom Vis Sci 2005;82:168-176.


10. Wolska A, Switula M. Luminance of the surround and visual fatigue of VDT operators. Int J Occup Saf Ergon 1999;5:553-581.


11. Han CC, Liu R, Liu RR, et al. Prevalence of asthenopia and its risk factors in Chinese college students. Int J Ophthalmol 2013;6:718-722.


12. Davey S, Davey A. Assessment of smartphone addiction in Indian adolescents: a mixed method study by systematic-review and meta-analysis approach. Int J Prev Med 2014;5:1500-1511.


13. Nathan N, Zeitzer J. A survey study of the association between mobile phone use and daytime sleepiness in California high school students. BMC Public Health 2013;13:840



14. Logaraj M, Madhupriya V, Hegde S. Computer vision syndrome and associated factors among medical and engineering students in Chennai. Ann Med Health Sci Res 2014;4:179-185.



15. Benedetto S, Drai-Zerbib V, Pedrotti M, et al. E-readers and visual fatigue. PLoS One 2013;8:e83676



16. Kawashima M, Yamatsuji M, Yokoi N, et al. Screening of dry eye disease in visual display terminal workers during occupational health examinations: the Moriguchi study. J Occup Health 2015;57:253-258.


17. Roh HC, Lee JK, Kim M, et al. Systemic comorbidities of dry eye syndrome: the Korean National Health and Nutrition Examination Survey V, 2010 to 2012. Cornea 2016;35:187-192.


18. Portello JK, Rosenfield M, Chu CA. Blink rate, incomplete blinks and computer vision syndrome. Optom Vis Sci 2013;90:482-487.


19. Bababekova Y, Rosenfield M, Hue JE, Huang RR. Font size and viewing distance of handheld smart phones. Optom Vis Sci 2011;88:795-797.


20. Tosini G, Ferguson I, Tsubota K. Effects of blue light on the circadian system and eye physiology. Mol Vis 2016;22:61-72.


21. Lee JB, Kim SH, Lee SC, et al. Blue light-induced oxidative stress in human corneal epithelial cells: protective effects of ethanol extracts of various medicinal plant mixtures. Invest Ophthalmol Vis Sci 2014;55:4119-4127.


22. Niwano Y, Kanno T, Iwasawa A, et al. Blue light injures corneal epithelial cells in the mitotic phase in vitro. Br J Ophthalmol 2014;98:990-992.

23. Jaadane I, Boulenguez P, Chahory S, et al. Retinal damage induced by commercial light emitting diodes (LEDs). Free Radic Biol Med 2015;84:373-384.


24. Oh JH, Yoo H, Park HK, Do YR. Analysis of circadian properties and healthy levels of blue light from smartphones at night. Sci Rep 2015;5:11325



25. Ide T, Toda I, Miki E, Tsubota K. Effect of blue light-reducing eye glasses on critical flicker frequency. Asia Pac J Ophthalmol (Phila) 2015;4:80-85.


26. Haug S, Castro RP, Kwon M, et al. Smartphone use and smartphone addiction among young people in Switzerland. J Behav Addict 2015;4:299-307.



27. Kim J, Hwang Y, Kang S, et al. Association between exposure to smartphones and ocular health in adolescents. Ophthalmic Epidemiol 2016;23:269-276.


28. Acosta MC, Gallar J, Belmonte C. The influence of eye solutions on blinking and ocular comfort at rest and during work at video display terminals. Exp Eye Res 1999;68:663-669.


29. Uchino M, Yokoi N, Uchino Y, et al. Prevalence of dry eye disease and its risk factors in visual display terminal users: the Osaka study. Am J Ophthalmol 2013;156:759-766.


Table 2
Asthenopia questionnaire form

Modified from the original version proposed by Ames et al. Optom Vis Sci 2005;82:168-76 [9].
- TOOLS
-
METRICS

-
- 64 Crossref
- 0 Scopus
- 4,114 View
- 99 Download
- Related articles



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



