Dear Editor,
Corneal blood staining can occur as a complication of traumatic hyphema with frequencies of 2% to 11%, particularly in the conditions of total hyphema, rebleeding, high intraocular pressure (IOP), and endothelial dysfunction [1,2]. Surgical interventions are recommended in eyes with high IOP and sustained blood in the anterior chamber to decrease the incidence of complications [3,4]. We describe the natural history of corneal blood staining following traumatic hyphema in an 8-year-old boy by presenting serial photography of the spontaneous clearance process.
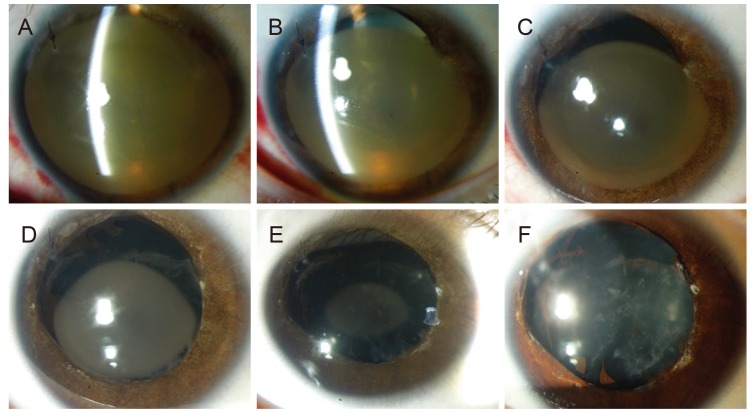
An 8-year-old boy visited Seoul St. Mary's Hospital with decreased visual acuity (VA) and corneal opacity after blunt trauma to the right eye 30 days prior. He had undergone irrigation of the anterior chamber for increased IOP combined with hyphema occupying over 90% of the anterior chamber at another hospital on the 6th day after trauma. There were no descriptions of cataract formation at that point. VA was reduced to hand-motion and IOP was 8 mmHg at the initial visit to our hospital (1-month post-trauma). Slit lamp examination revealed rust-colored corneal opacity occupying the entire cornea, which obscured the iris, lens, and posterior segment (Fig. 1A). The affected cornea was mildly edematous, and central corneal thickness was 703 ┬Ąm. Two months after the trauma, the blood-stained area seemed to clear from the peripheral limbus (Fig. 1B) with slight improvement in VA, so we chose to follow-up regularly instead of performing any invasive intervention. At post-traumatic 3 months, the diameter of the blood-stained area had decreased and the patient was prescribed partial-patch of the left eye (Fig. 1C). Centripetal clearance had continued to improve at 6 months, with VA at 20 / 100 (Fig. 1D). He was prescribed myopic glasses with maintenance of occlusion therapy. VA was corrected to 20 / 40 with a 2.5 ├Ś 3.0-mm-sized central discoid lesion at 12 months (Fig. 1E). The fundus was clearly visible at that time. Complete corneal clearance was achieved, and he showed a final VA of 20 / 40 at 15 months (Fig. 1F). Traumatic mydriasis and cataract remained. Corneal endothelial cell density was 1,282 cells/mm2. No stromal or endothelial opacities were detected in the affected eye.
Corneal blood staining usually occurs in the setting of large persistent hyphema, increased IOP, and corneal endothelial cell dysfunction [1,2]. Hemoglobin is released from erythrocytes into the anterior chamber. Increased IOP may aggravate stromal penetration of hemoglobin and its breakdown products through the endothelium whose barrier function has been anatomically and physiologically compromised. Hemoglobin and its breakdown products aggregate within the stromal lamellae and are phagocytized and metabolized by keratocytes, which then produce intracellular hemosiderin [1,2].
The corneal blood staining cleared without any permanent corneal opacities in the present 8-year-old boy even though the total clearing process lasted 15 months. Decreased endothelial cell density could be caused by either mechanical disruption of the endothelium or photosensitization of the endothelium by hemoglobin-derived porphyrins [5]. A VA of 20 / 40 was achieved with aggressive optical correction and occlusion therapy during the clearing process. Regarding traumatic lens opacity, cataract surgery can be considered for further improvement in VA. As demonstrated in Fig. 1, the clearance process occurred from the periphery toward the center with an abrupt demarcation line between the cleared and stained corneal stroma. McDonnell et al. [2] have suggested that the primary mechanisms responsible for clearing hemoglobin and its products are diffusion toward the limbal circulation and within the anterior chamber and shedding of iron-containing epithelial cells. Corneal clearing has been reported to be accomplished within 3 years in most cases, although duration varies. [1,4].
In particular, corneal blood staining after resolution of hyphema can lead to deprivation amblyopia in children during visual development. Preventing corneal blood staining is most important by surgically evacuating the blood clot in children with hyphema and early recognition of the first signs of microscopic corneal blood staining, including straw yellow discoloration and the presence of tiny yellowish granules in the deep stroma [3,4]. Pediatric ophthalmologists treating children with corneal blood stains should consider the density and area of the corneal lesion, patient age, and the time required for total clearing when making a choice between waiting for spontaneous clearance or performing penetrating keratoplasty. Favorable final VA can be achieved through appropriate refractive correction and occlusion therapy.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






