Dear Editor,
Local anesthesia with an epinephrine-lidocaine mixture has been widely used in cosmetic facial procedures and oculoplastic surgery. Although the known side effects of local anesthesia include pain and hematoma in the injected area, we encountered a case of atypical ophthalmic artery occlusion (OAO) after subcutaneous injection of an epinephrine-lidocaine mixture into the supratrochlear area.
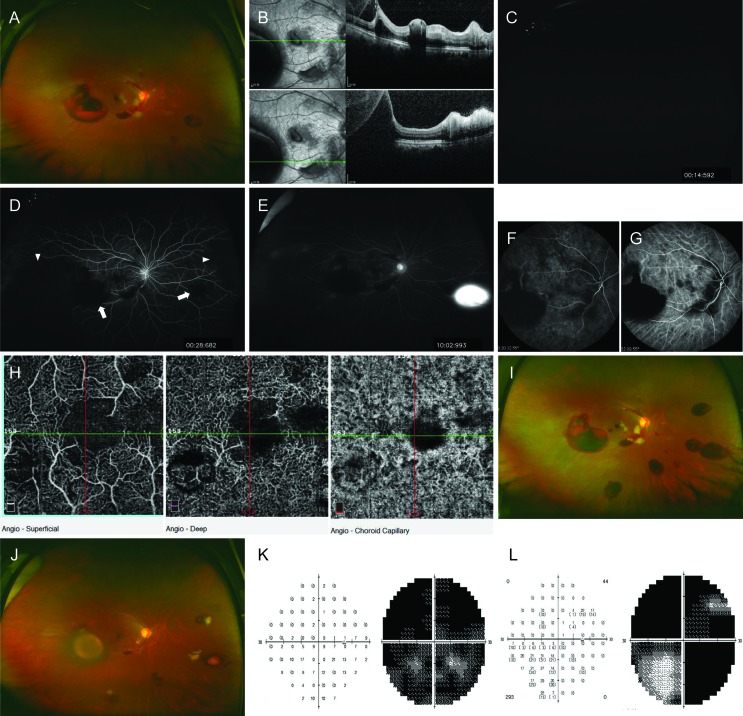
A 47-year-old woman complained of sudden visual disturbances in her right eye, which had developed 3 days earlier. The best-corrected visual acuity was 0.03, and a grade-II afferent pupillary defect was observed. Upon slit lamp examination, many red blood cells were found in the anterior chamber. Fundus examination revealed cotton wool patches (CWPs) of various sizes, and retinal hemorrhages at the posterior pole. Moreover, large preretinal hemorrhages were observed (Fig. 1A). Optical coherence tomography revealed hyperreflectivity in the inner retinal layer and multiple preretinal hemorrhages (Fig. 1B). Fluorescein angiography displayed slightly delayed chorioretinal filling, definite peripheral nonperfusion areas at the nasal and temporal periphery and vascular leakage and staining (Fig. 1C-1E).
The patient was relatively healthy before the episode. However, 3 days earlier, she had visited a local cosmetic clinic for facial filler injection and, before the procedure, received a subcutaneous injection containing 1 : 100,000 epinephrine and 2% lidocaine in the right supratrochlear area. She reported that it was the first injection in the procedure. Immediately after the injection, severe ocular pain, a thunder-like entoptic phenomenon, mydriasis, ptosis, and visual disturbances developed. She visited an emergency clinic and was diagnosed with central retinal artery occlusion (CRAO). Indocyanine green angiography revealed hypoperfusion of the choroidal arteries and choriocapillaris (Fig. 1F and 1G). Furthermore, optical coherence tomography angiography showed capillary loss in all retinal layers and in the choriocapillaris (Fig. 1H). We suspected that epinephrine had induced atypical OAO, and treated this patient with high-dose corticosteroid therapy for 3 days. Thereafter, the retinal hemorrhages increased in size and number and changed in shape (Fig. 1I). Four weeks after the initiation of treatment, most of the retinal hemorrhages and CWPs had been absorbed (Fig. 1J); however, count-fingers vision persisted and the visual field defect was not resolved (Fig. 1K and 1L).
Epinephrine acts peripherally on ╬▒-adrenergic receptors, resulting in the constriction of blood vessels [1]. Previous reports have described embolic occlusion caused by various materials, such as fillers or autologous fat. These materials can cause CRAO, OAO and/or cerebral infarction [2]. However, our particular patient had not received a filler injection, and her symptoms differed from the more devastating symptoms of filler-associated OAO, which include no recovery of light perception, visible filler material with arterial segmentation, and more complete chorioretinal artery filling defects on fluorescein angiography or indocyanine green angiography [3]. We suspect that other factors related to the epinephrine injection contributed to the development of this case. First, there were various changes in the clinical course of the disease, given that many of the initial signs of OAO had disappeared after 3 days. Furthermore, the CRAO-like fundus characteristics changed to retinal hemorrhages, CWPs, and peripheral nonperfusion areas. Although preretinal hemorrhage is not a characteristic finding of OAO, we think that the injected materials migrated in the anterograde direction and then induced peripheral vascular constriction and spasm, which contributed to peripheral nonperfusion, vascular leakage and preretinal hemorrhage caused by vessel wall damage. Second, epinephrine can cause visual disturbances including diplopia following trigeminal nerve block during dental procedures or following local anesthesia of the nasal mucosa during nasal surgery [4,5]. The proposed mechanism of transient OAO in these instances is vascular spasm resulting from intra-arterially injected epinephrine with retrograde migration. Finally, to the best of our knowledge, there have been no reported cases of OAO secondary to subcutaneous injection of local anesthetics alone. Thus, in our case, retrograde arterial displacement of the injected epinephrine from a branch of the supratrochlear artery into the ophthalmic arterial system may have blocked the ophthalmic artery immediately after injection. Through vasodilation over time, subsequent anterior movement of epinephrine to more distal vessels may have led to vasoconstriction and subsequent vasospasm.
In conclusion, epinephrine can lead to OAO following accidental intra-arterial injection of subcutaneously administered local anesthetics. Hence, physicians should carefully administer local anesthesia while considering the possibility that such a complication may occur.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






