 |
 |
| Korean J Ophthalmol > Volume 31(2); 2017 > Article |
Dear Editor,
Jung et al. [1] are to be congratulated on definitively demonstrating what could only be surmised in the pastŌĆöthat intraocular angiogenesis after central retinal artery occlusion (CRAO) occurs in that small proportion of cases wherein retinal reperfusion fails to materialize [2,3]. However, your contributors appear to be unsure as to the mechanism whereby neovascularisation of the iris (NVI) arises after ŌĆ£CRAO alone.ŌĆØ While they reject Hayreh's [4] assertion that ŌĆ£chronically hypoxic retina ... is totally missingŌĆØ after what is otherwise called ŌĆ£isolated CRAOŌĆØ (and implicating ocular ischemia in NVI development due, for example, to carotid arterial stenosis), the crucial link between isolated CRAO and NVI was not elucidated.
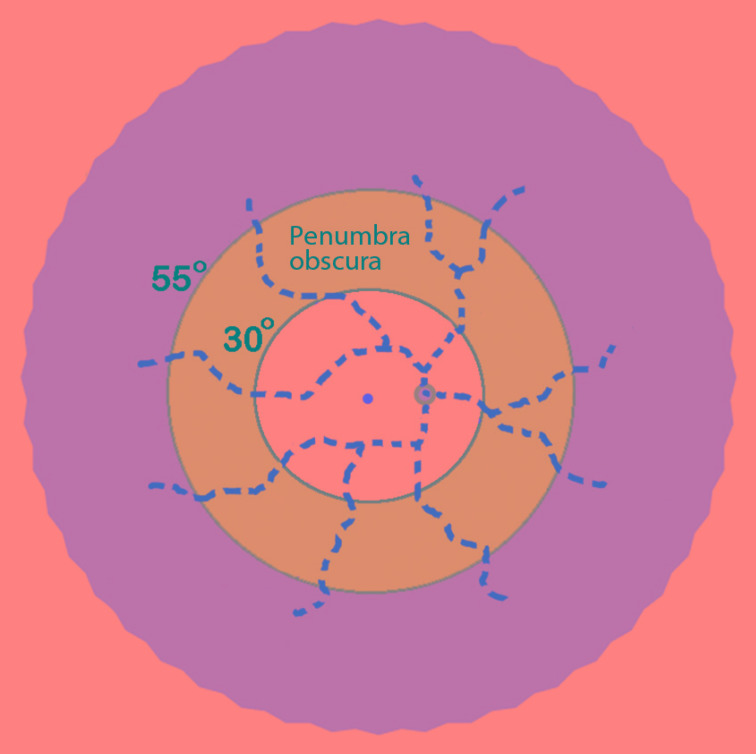
In reality, there is a perfectly straightforward explanation for NVI after isolated CRAO that entirely resonates with Jung et al.'s findings. A recent review of the electrophysiological data from legacy experiments in primates has shown that a transparent mid-peripheral hypoxic tissue compartment-the ŌĆ£penumbra obscuraŌĆØ-evolves within the inner retina after CRAO (Fig. 1) and surrounds the opacified anoxic infarct in the posterior pole [3]. The penumbra obscura is marginally oxygenated by the choroid and is analogous to the ischemic penumbra that surrounds the infarct core in cerebral stroke. After cerebral arterial occlusion, however, penumbra-to-umbra conversion takes place within approximately 6 hours of ischemia onset, with incorporation of most if not all of the penumbral cortex into the infarct. By contrast, the hypoxic swathe in the retina endures and secretes pro-angiogenic molecules such as vascular endothelial growth factor (VEGF). Furthermore, neovascularisation within the eye is not self-limiting in nature, in contrast to angiogenesis elsewhere, because the (iris) neovascular response is remote from the (retinal) hypoxic source [5]. In other words, the penumbra obscura does not become revascularized as part of the angiogenic process.
Although the link between CRAO and NVI is readily apparent, final proof of concept is still lacking (e.g., by demonstration of VEGF secretion from the penumbra obscura in eyes enucleated for rubeotic glaucoma secondary to CRAO). In the meantime, all eyes with complete CRAO and diffuse opacification in the posterior pole should be considered to be ŌĆ£at riskŌĆØ of intraocular angiogenesis. However, the majority of eyes with CRAO will undergo spontaneous or therapeutic CRA recanalization and inner retinal reperfusion, resulting in hypoxia-to-normoxia conversion within the penumbra obscura and cessation of VEGF secretion. As Jung et al. [1] point out, therefore, documentation of retinal reperfusion by fluorescein angiography (or other means) dictates that close follow-up of the patient for signs of NVI is no longer necessary. Theoretically, the volume of the penumbra obscura (and the risk of rubeosis iridis) will also be reduced if there is associated posterior ciliary arterial occlusion (e.g., due to cranial arteritis) since penumbral (hypo-)oxygenation by the choroid will be compromised. This may help to explain Jung et al.'s [1] observation of eyes with failed CRA recanalization but no NVI.
Finally, the traditional view that intraocular angiogenesis is characteristic of retinal venous occlusion (with permanent capillary non-perfusion) no longer holds true. Retinal arterial occlusions are equally capable of initiating an angiogenic response, although arteriovenous shunt vessels crossing non-perfused inner retina may give rise to an additional pro-angiogenic source after vein occlusion. As already noted, blood flow through the inner retinal microcirculation frequently recovers after CRAO (courtesy of arterial recanalization), with resulting abolition of the angiogenic stimulus from the penumbra obscura [3]. After venous occlusion, there is an ongoing debate as to the number of disc areas of retina that must be involved in irreversible capillary closure before NVI is initiated, but the risk of rubeosis depends on the site of that closure (in relation to the penumbra obscura) as well as its dimension. Also of note, a localised area of permanent capillary closure is sometimes seen in the central macular region after clinical CRAO and recanalization-a phenomenon called ŌĆ£no-reflow [4].ŌĆØ However, this is an epiphenomenon in that the whole of the inner retina in the posterior pole (extending to Ōēł30┬░ eccentricity from the fovea) undergoes anoxic infarction in such eyes [3]. Thus, this central no-reflow zone is irrelevant to the development of NVI after CRAO. Instead, non-reperfused hypoxic inner retina between Ōēł30┬░ and Ōēł55┬░ eccentricity from the fovea (Fig. 1) serves as the essential pro-angiogenic source [3,5].
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Jung YH, Ahn SJ, Hong JH, et al. Incidence and clinical features of neovascularization of the iris following acute central retinal artery occlusion. Korean J Ophthalmol 2016;30:352-359.



2. Duker JS, Brown GC. Iris neovascularization associated with obstruction of the central retinal artery. Ophthalmology 1988;95:1244-1250.


Fig.┬Ā1
Schematic diagram of oxygenation-based tissue compartments in the inner retina after central retinal artery occlusion (pink, normoxic periphery; pale blue, hypoxic mid-periphery; unshaded/white, anoxic posterior pole (as in references [3] and [5]). The penumbra obscura lies between threshold oxygen tension isobars at Ōēł30┬░ and Ōēł55┬░ eccentricity from the foveolar cherry-red spot. Dashed red lines emanating from the optic disc signify cattle-trucking in the central arterial tree.
Author reply
Dear Editor,
I greatly appreciate David McLeod for his interest and helpful comments on our article entitled ŌĆ£Incidence and clinical features of neovascularization of the iris following acute central retinal artery occlusion [1].ŌĆØ He clearly explained the mechanism of ocular neovascularization after central retinal artery occlusion (CRAO) and highlights the insight of retinal ŌĆ£ischemic penumbraŌĆØ as the source of angiogenic factors leading to ocular neovascularization. In his present comment as well as in his prior review article [2], he elaborates the detailed features of ischemic penumbra in CRAO: a hypoxic compartment or retinal area that is functionally silent but has not fallen into infarction. In classic CRAO, the hypoxic retinal ischemic penumbra is the mid-periphery between the anoxic posterior pole and the normoxic peripheral retina. In most part, I agree with his explanation on the mechanism that the angiogenic factors secreted from the surviving hypoxic cells in the ischemic penumbra cause the ocular neovascularization. However, the experimental data using primates did not completely reflect this situation of chronic CRAO without reperfusion; thus, there are still unanswered questions. Specifically, what is the retinal area of ischemic penumbra in chronic CRAO? On optical coherence tomography images of CRAO 1 year after the initial event, we can see remnant inner retinal tissues in the posterior pole [3]. I agree that, in the acute stage of CRAO, the posterior retina with cherry-red opacification is in an anoxic condition and has fallen into infarction. But, in the later chronic stage without arterial reperfusion, the area of the ischemic penumbra may comprise the posterior pole where residual inner retinal neurons are still present, although most of the inner retinal cell mass has disappeared due to acute anoxic infarction. In addition, the retinal thinning after acute CRAO attack could reduce the oxygen consumption by the inner retinal neurons, which could constrict the area of ischemic penumbra in chronic CRAO. In addition, if the ischemic penumbra persists immediately after acute CRAO attack, why is the ocular neovascularization observed after 3 months (on average) of occlusion [1]? Currently, there is no precise experimental model for chronic CRAO, and these issues remain to be elucidated further.
The value of intra-arterial thrombolysis or fibrinolysis for visual recovery is minimal considering the cortical deafferentation by the infarcted ganglion cell axons in the posterior pole and papillomacular bundles [2,4]. However, the higher rate of early anatomic recanalization by thrombolysis [5] suggests that this intervention may reduce the incidence of ocular neovascularization and its complications. Currently, therefore, it may be too early to discard the option of intra-arterial thrombolysis for CRAO, and this debate needs further investigation.
In conclusion, ocular neovascularization, such as iris neovascularization and neovascular glaucoma, actually occurs in a small proportion (about 10%) of eyes with central retinal artery occlusion irrespective of carotid artery stenosis. This complication develops only in eyes with failed arterial reperfusion, namely, chronic CRAO. Ophthalmologists should know that this serious complication can develop following CRAO attack, and it should be monitored carefully with regular fundus fluorescein angiography.
REFERENCES
1. Jung YH, Ahn SJ, Hong JH, et al. Incidence and clinical features of neovascularization of the iris following acute central retinal artery occlusion. Korean J Ophthalmol 2016;30:352-359.



2. Duker JS, Brown GC. Iris neovascularization associated with obstruction of the central retinal artery. Ophthalmology 1988;95:1244-1250.





 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




