 |
 |
| Korean J Ophthalmol > Volume 30(6); 2016 > Article |
Dear Editor,
Anterior transposition of the inferior oblique (IO) muscle is an effective treatment for dissociative vertical deviation (DVD) when associated with IO muscle overaction [1]. By transposing the insertion of the IO muscle anterior to the equator, a force vector of the IO muscle converts from elevation to depression, which in turn reduces DVD [1]. After the procedure, the superior rectus muscle has a partial abducting vector, and the lateral rectus muscle has a partial vector for depression, secondary to the substantial residual extorsion [2]. This procedure can cause limitations of elevation in abduction in the operated eye as well as marked upshoot of the contralateral adducting eye that mimics recurrent or new overaction of the IO muscle of the other eye. This adverse outcome has been named the antielevation syndrome [3]. The antielevation syndrome has been shown to occur more frequently if the new insertion of the IO muscle is placed anterior to the inferior rectus muscle insertion or if the posterior lateral fibers of the IO muscle are spread out substantially rather than bunched up with the anterior nasal corner. It is also more likely to occur if some of the IO muscle is resected inadvertently by suture placement proximal to the insertion [3]. We report a long-standing antielevation syndrome with a V pattern exotropia following bilateral anterior transposition of IO muscles.
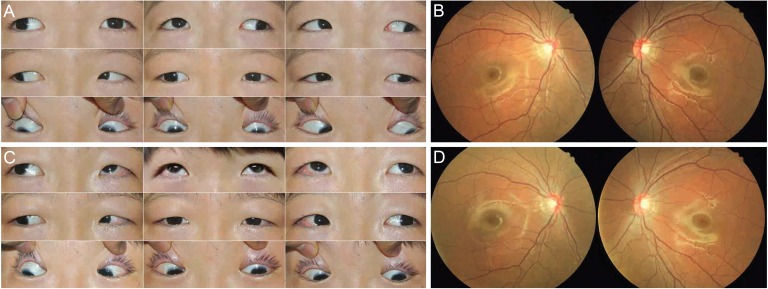
An 11-year-old boy, who had a history of bilateral anterior transposition of the IO muscles for bilateral IO overaction at 2 years of age at another hospital, presented at Konyang University Hospital for intermittent exotropia with an abnormal ŌĆśchin-upŌĆÖ head position. He had a significant 40 prism diopters (PD) exotropia and 6 PD right hypotropia in the primary position that increased to 50 PD exotropia on upgaze and improved to 20 PD exotropia in downgaze. The right hypotropia was 20 PD in the straight right gaze and was reversed to 14 PD for the left hypotropia in the straight left gaze. On the extraocular motility examination, there were limitations of elevation in abduction of -4 and an IO muscle overaction of +4 in both eyes (Fig. 1A). Fundus photography revealed severe excyclotorsion in both eyes (Fig. 1B). Antielevation syndrome was suspected and treated with bilateral extirpation without denervation of IO muscles and a bilateral lateral rectus recession of 8.0 mm. Intraoperatively, there were mild adhesions between the IO muscles and the surrounding tissues; the anterior fibers of the IO muscle were placed 3 mm anterior to the inferior rectus insertion of the right eye and 2 mm anterior to the inferior rectus insertion of the left eye; and the posterior fibers were identified 3 mm lateral to the anterior fibers, but there was no restriction on forced duction testing of both eyes. At 3 months postoperatively, there was a remaining exotropia of 16 PD, but limitations of elevation, IO overaction of both eyes, abnormal ŌĆśchin-upŌĆÖ head position and excyclotorsion in both eyes improved (Fig. 1C and 1D). Also, there was no significant DVD, postoperatively.
The limitation of elevation in the operated eye and marked upshoot of the contralateral adducting eye secondary to the restriction of elevation of the abducting eye on upgaze may cause vertical strabismus in the primary position and create a V or Y pattern [3]. Antielevation syndrome as an adverse outcome of anterior transposition of the IO muscle is usually known to appear in the early postoperative period. However, antielevation syndrome is not frequently present initially after IO anterior transposition, but instead can develop several years later. Kushner [2] reported two patients who developed the anti-elevation syndrome long after surgery. Denervation-extirpation of IO muscle and IO nasal myectomy can successfully treat antielevation syndrome [3,4,5]. Mims and Wood [4] reported that bilateral nasal myectomy is preferable to denervation-extirpation because denervation-extirpation can unleash significant DVD. The optimum surgical treatment for long-standing antielevation syndrome after anterior transposition of the IO muscle has yet to be decided. In this case, we achieved successful result with extirpation without denervation of bilateral IO muscles with long-standing antielevation syndrome after bilateral anterior transposition of the IO muscles to correct limitation in elevation, and excyclotorsion.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Scott AB. Planning inferior oblique muscle surgery. In: Reinecke RD, Strabismus. New York: Grune and Stratton; 1978. p. 347-354.
2. Kushner BJ. Torsion as a contributing cause of the anti-elevation syndrome. J AAPOS 2001;5:172-177.


3. Kushner BJ. Restriction of elevation in abduction after inferior oblique anteriorization. J AAPOS 1997;1:55-62.


Fig.┬Ā1
(A) Preoperative clinical photographs. Ocular motility examination showed limitation in elevation, higher on the abduction than adduction of both eyes. (B) Preoperative fundus photographs. The photos showed severe excyclotorsion of both eyes. (C) Clinical photographs 3 months after extirpation of the both inferior oblique muscles and bilateral lateral rectus muscle recession. Ocular motility examination showed improvement of elevation in abduction position of both eyes. (D) Fundus photographs 3 months postoperatively, the excyclotorsion of both eyes had improved.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




