Visual Outcomes Following Deep Anterior Lamellar Keratoplasty in Granular Corneal Dystrophy Types 1 and 2
Article information
Dear Editor,
The phenotypic appearance of granular corneal dystrophy (GCD) type 1 and GCD type 2 (also known as Avellino corneal dystrophy) changes with age, but is believed to also be influenced by trauma or intervening surgical procedures [123]. This report presents two cases of GCD, with varied manifestations before and after surgical intervention. Incidentally, Lee et al. [4] noted high prevalence Avellino dystrophy in the Korean population, approximately 11.5 of 10,000.
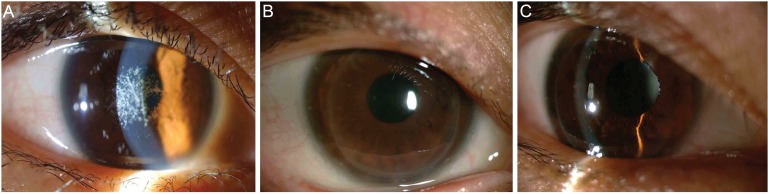
A 55-year-old Caucasian male with GCD type 1 in 2008 initially presented with deteriorating visual acuity (VA) following an anterior lamellar keratoplasty in the left eye (LE) in 1999 (Fig. 1A). His sister was also diagnosed with GCD type 1. Slit lamp examination showed bilateral granular opacities with the granules in the LE, located mainly in the graft host interface. VA in the right eye (RE) was 6 / 30 unaided, 6 / 21 with a pinhole, and in the LE was 6 / 120 unaided, 6 / 18 with a pinhole. He underwent a deep anterior lamellar keratoplasty (DALK) 6 months after presentation in the RE, and 15 months in the LE. Following suture removal from both grafts, the VA in the RE was 6 / 15 unaided, correcting to 6 / 7.5 (28 months post-DALK), and in the LE was 6 / 18 unaided, correcting to 6 / 6 (20 months post-DALK). Minor recurrence of the granular dystrophy at the graft host interface was noted bilaterally 25 months post-left DALK (Fig. 1B and 1C). Fifty-seven months after the right and 48 months after the left DALK, the VAs were 6 / 7.5 bilaterally with correction.

Case 1. (A) Slit lamp image of left eye showing lamellar keratoplasty with recurrence of the granular deposits in the graft host interface, (B) image of left eye 52 months post-deep anterior lamellar keratoplasty with full graft shown, and (C) slit lamp image of left eye 52 months post-deep anterior lamellar keratoplasty showing minor recurrence of granular deposits at the graft host interface.
A 27-year-old Korean female in 2008, 8 years subsequent to bilateral laser-assisted in situ keratomileusis (LASIK), presented with changes consistent with granular dystrophy around the LASIK interfaces (Fig. 2A). Her mother, sister, maternal uncle, and multiple maternal cousins were all diagnosed with some form of corneal dystrophy. Further DNA assessment led to a definitive diagnosis of Avellino dystrophy.
Case 2. (A) slit lamp image of right eye post-laser-assisted in situ keratomileusis showing granular and lattice deposits characteristic of Avellino corneal dystrophy, (B) image of right eye post-deep anterior lamellar keratoplasty with graft clearly shown, and (C) slit lamp image of right eye post-deep anterior lamellar keratoplasty showing slit lamp beam through clear corneal graft.
At the initial visit, the VA was 6 / 15 with glasses, and anterior stromal granules were noted on slit lamp examination. The RE preoperative VA was 6 / 15 with correction. She underwent DALK to the RE 18 months after presentation. Following suture removal, 14 months after the right DALK, VA was counting fingers, improving to 6 / 48 with a pinhole, and the graft was clear at 36 months. Fifty-five months post-DALK, VA was 6 / 18, improving to 6 / 15 with a pinhole and a clear graft (Fig. 2B and 2C).
At the initial visit, VA was 6 / 18 with glasses, improving to 6 / 15 with a pinhole, and posterior stromal granules were noted. LE VA preoperatively was 6 / 15 with glasses and improved to 6 / 12 with the pinhole. She underwent left DALK 49 months after presentation. The VA at the last appointment was 6 / 15 with glasses, with no improvement with a pinhole and a clear graft.
On first presentation, slit lamp examination of case 1 showed bilateral granular opacities, with those in the LE largely located at the existing graft-host interface. Following bilateral DALK, minor recurrence of granules was noted at the graft-host interface. Recurrence in the graft-host interface following DALK and lamellar keratoplasty is noted in the literature, and often granules will progress over time from the epithelium to the stroma [4]. Disease recurrence is well recognized in the graft-host interface area, and may be related to both GCD types, as well as surgical factors such as recurrence along suture tracks and incision lines [12345]. The exact reasons why recurrence is seen in some cases and not in others has yet to be elucidated.
Both current cases showed excellent improvement in VA (6 / 7.5 in case 1 and approximately 6 / 15 in case 2). In general, VA improvement is expected after DALK, although it has been reported to range between 6 / 7.5 and 6 / 120 [5]. Slit-lamp examination of case 2 demonstrated multiple granules in the stroma anterior to and surrounding the flap, 8 years post-LASIK. Awwad et al. [1] suggest that LASIK results in exacerbation of Avellino dystrophy deposits in the flap interface and in the stroma anterior to the interface.
Clinicians must be aware that current refractive corneal surgeries such as LASIK are contraindicated in granular corneal dystrophies, as they induce progression of the disease, and case 2 appears to support this statement [3].
Currently, DALK remains the best treatment option for improving VA in patients with granular corneal dystrophies, even if repeat procedures are required. These cases demonstrate that positive VA outcomes are achievable in typical GCD types 1 and 2.
Acknowledgements
We would like to thank professor Charles NJ McGhee for his input and oversight.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.