Dear Editor,
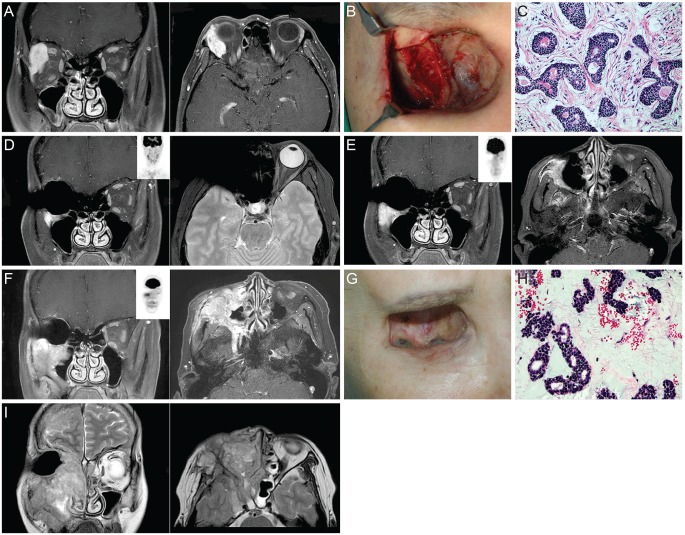
This report describes a patient with locally aggressive adenoid cystic carcinoma (ACC) of the lacrimal gland that recurred after neoadjuvant intra-arterial chemotherapy (IAC), local surgery and postoperative radiotherapy. A 47-year-old female presented with painless swelling of her right eyelid that had persisted for 3 months. Physical examination revealed 3-mm exophthalmos of the right eye. Orbit magnetic resonance imaging (MRI) with contrast revealed an approximately 3-cm-sized enhancing lesion in the right lacrimal gland with bony invasion (Fig. 1A). Incisional biopsy verified ACC. Neoadjuvant intracarotid adriamycin and cis-platinum was started, but the patient was switched to the intravenous regimen due to facial swelling and tenderness. After two chemoreduction cycles, the patient underwent orbital exenteration. Because the resected margin of the lateral exenterated orbit and zygoma were positive for carcinoma, additional lateral zygoma bone was removed (Fig. 1B). The pathology report verified T4bN0M0 stage ACC, cribriform type, with lymphovascular invasion (Fig. 1C). The patient then received postoperative 59.4 Gy radiotherapy. An MRI taken 1 year after exenteration revealed an approximately 7-mm, focal enhancing lesion in the right anterior maxilla bone, suggestive of possible tumor recurrence. However, positron emission tomography-computed tomography (PET-CT) did not show increased uptake of fludeoxyglucose (FDG) (Fig. 1D). The patient refused to have a bone biopsy. A repeat MRI performed 2 years after surgery indicated that there was an increase in the extent of the enhancing lesion inferior to the right orbit and right pterygomaxillary fissure and suspicious tumor spread along the right foramen rotundum, but again no increased FDG uptake was observed on PET-CT (Fig. 1E). A bone biopsy was recommended which the patient refused. A PET-CT taken 3 years postoperatively again showed a stable disease state, however, the patient presented with an elevated pigmented mass along the inferolateral margin of the exenterated orbit after 6 months. An MRI revealed a markedly increased infiltrating mass along the entire maxillary sinus wall with perineural spread to the cavernous sinus via the foramen rotundum. At that time, PET-CT finally showed consistent findings of high FDG uptake (Fig. 1F). An excisional biopsy of the elevated pigmented lesion (Fig. 1G) confirmed the pathology as recurred ACC (Fig. 1H). The patient was referred to the head and neck surgery department and a salvage operation was planned, however the patient refused to undergo the operation and she did not return until she presented to the emergency room in a confused mental status with blindness in her left eye a year later. An MRI revealed an increased right maxillary sinus mass with intracranial extension, brain edema, and infiltration into the left orbital apex compressing the optic nerve (Fig. 1I). Upon refusal of further treatment, the patient died within 1 month.
ACC is an aggressive malignant neoplasm with locoregional recurrence being the most common cause of disease progression and death [1]. Surgery and radiotherapy are the conventional treatment modalities, but whether the addition of IAC improves survival and whether the risk of potential toxicities should be taken remain controversial. Tse et al. [2] reported that the cumulative 5-year carcinoma cause-specific death rate was 16.7% in the group treated with IAC and exenteration. In contrast, Fellman et al. [3] reported 2 cases of ACC recurrence and distant metastasis after IAC followed by surgery and high-dose radiation therapy. We report a case of recurring ACC that involved the contralateral eye and brain, despite multimodality treatment. The condition was not detectable on PET-CT scan for several years. ACC has been reported to be FDG avid, manifesting low FDG uptake compared to size-matched squamous cell carcinoma [4]. Cribriform or tubular histologic subtypes show even lower FDG uptake compared to the solid pattern, and therefore physicians should be meticulous when interpreting PET-CT results in ACC patients.
The locally aggressive nature of the cancer and the inconsistent radiologic findings [5] which was apparent in this case highlight the need for serial MRI follow-up for monitoring of disease progression, for prompt biopsy when recurrence is suspected, and for radical local control of the disease. Also, the potential complications of IAC, such as facial tenderness and swelling that were experienced by our patient, and other factors that lead to the optimal treatment response, should be taken into consideration when deciding the treatment regimen for ACC.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






