 |
 |
| Korean J Ophthalmol > Volume 29(5); 2015 > Article |
Abstract
Purpose
We present clinical results of the use of the multipurpose conical porous synthetic orbital implant (MCOI) in surgical procedures of evisceration, enucleation, and secondary enucleation in ophthalmology patients.
Methods
A retrospective review was performed of 59 eyes in which conical implants were used, including 36 cases of eviscerations, 11 enucleations, and 9 secondary enucleations. In all of the cases, the follow-up period was greater than six months between 2004 and 2013. The results focus on documenting surgical findings, as well as postoperative complications among patients.
Results
Superior sulcus deformities were found in six eyes (10.2% of conical implant patients), and two eyes received additional surgical interventions to correct the deformities (3.4%). Blepharoptosis was found in four eyes (6.8%), two of which received upper eyelid blepharoplasty (3.4%). Fornix shortening was reported in only one eye (1.7%). Forty-one eyes had a satisfactory cosmetic appearance after the final prosthetic fitting of conical implants (69.5%). The most frequent postoperative complication was orbital implant exposure, which seemed to occur when the preoperative status of the conjunctiva, Tenon's capsule, and sclera preservation were poor in the eyes of the patients.
Conclusions
There was a lower incidence of blepharoptosis and fornix shortening with the MCOI in comparison to spherical implants, while the incidence of orbital implant exposure was similar with the MCOI in comparison to other types of orbital implants. In addition, the MCOI may have advantages with respect to postoperative cosmetic outcomes.
Evisceration and enucleation are surgical inevitabilities for some patients, even though the procedures have a lot of surgical and postoperative complications. These are the only treatment options for certain ocular diseases, including phthisis bulbi, endophthalmitis, and painful blind eye. While treatment options are limited by the status of the disease, certain postoperative complications, including enophthalmos, retraction of the upper eyelid, deepening of superior sulcus, migration of orbital implants, and shortening of the inferior fornix, cause further significant pain in patients who have already undergone considerable stress. These complications are associated with orbital volume deficiencies and the loss of surrounding supporting soft tissue, which occur secondary to globe removal [1].
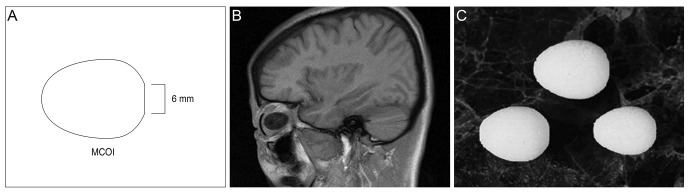
The multipurpose conical porous synthetic orbital implant (MCOI; Medpor, Porex Surgical, College Park, GA, USA) was designed to correct orbital volume deficiencies in patients requiring surgical implants. In contrast to traditional spherical orbital implants, the MCOI has a conical shape, with a wider and flattened anterior portion and a narrower and longer posterior portion. This shape makes the MCOI more similar to the natural anatomy of the orbital space (Fig. 1). The unique design of the MCOI enables the implant to replace more space in the conus and prevent lid deformities in patients undergoing treatment with implants [2]. The wider and flattened anterior portion prevents narrowing of the inferior fornix, and provides more space to cover the implant. The longer and narrower posterior segment is able to occupy more space, including the posterior portion of the conus. Furthermore, the synthetic porous polyethylene contains pores, allowing fibrovascular ingrowth, which reduces the incidence of orbital implant exposure and migration, as well as minimizes the rate of infection by allowing an immunological response within the implant [3,4].
Currently, there are only a limited number of reports on clinical outcomes of the use of MCOIs in patients undergoing ophthalmologic surgeries [2,5]. We expect that the MCOI may have advantages in cosmetic outcomes because of sufficient volume replacement after surgery. Here we report long-term clinical outcomes in patients after evisceration, enucleation and secondary enucleation performed using the MCOI over a nine-year period.
A retrospective review of medical charts was performed for 59 eyes in patients that underwent evisceration, enucleation, and secondary enucleation using an MCOI between 2004 and 2013 by a single surgeon, SW Yang, at Seoul St. Mary's Hospital. This study was approved by the institutional review board of the Catholic University of Korea. The patients signed a consent form confirming that they had been fully informed prior to the surgery. Only the patients who received follow-up care for longer than six months were included in our analysis, and patients with less than six months of follow-up care were excluded. Patient demographics (i.e., age and gender), reason for surgery, type of surgery, implant size, and postoperative complications were recorded. Enucleation was only performed when evisceration was contraindicated. An appropriately-sized MCOI (i.e., 16, 18, or 20 mm) was used to replace the eyes of each patient, as needed.
In enucleations of the patients herein, 360° peritomies were performed. Four rectus muscles were identified, isolated, and secured using locked 5-0 Vicryl (Ethicon, Somerville, NJ, USA). During continuation of posterior dissection, the superior and inferior oblique muscles were divided. Optic nerve transection was performed, and bleeding was controlled by hemostasis and monopolar diathermy. The appropriate implant size was determined for each eye using a sizing ball. The MCOI was kept in its sterile package and bathed in 10-mL saline with 80-mg gentamicin sulfate for 30 minutes. The implant was placed into the conal space, and the preserved rectus muscles were sutured directly to the implant. The Tenon's capsule and conjunctiva were sutured using 6-0 Vicryl (Ethicon).
In the eviscerations reviewed herein, 360° peritomies were performed, and a scleral incision was made circumferentially 1 to 2 mm apart from the limbus. Uveal tissue was separated from the scleral shell using an evisceration spoon, and the globe contents were removed. The inner side of the globe was cleaned and debrided using a gauze swab, and an anterior relaxing incision was made. An additional relaxing incision was performed circumferentially at the equatorial level, and the appropriate orbital implant size was determined using the same method as in enucleation. The scleral shell was closed using 5-0 Vicryl, and the Tenon's capsule and conjunctiva were sutured using 6-0 Vicryl. Following surgery, a conformer was inserted, and antibiotic ointment was applied to the ocular surface to prevent wound dehiscence and infection.
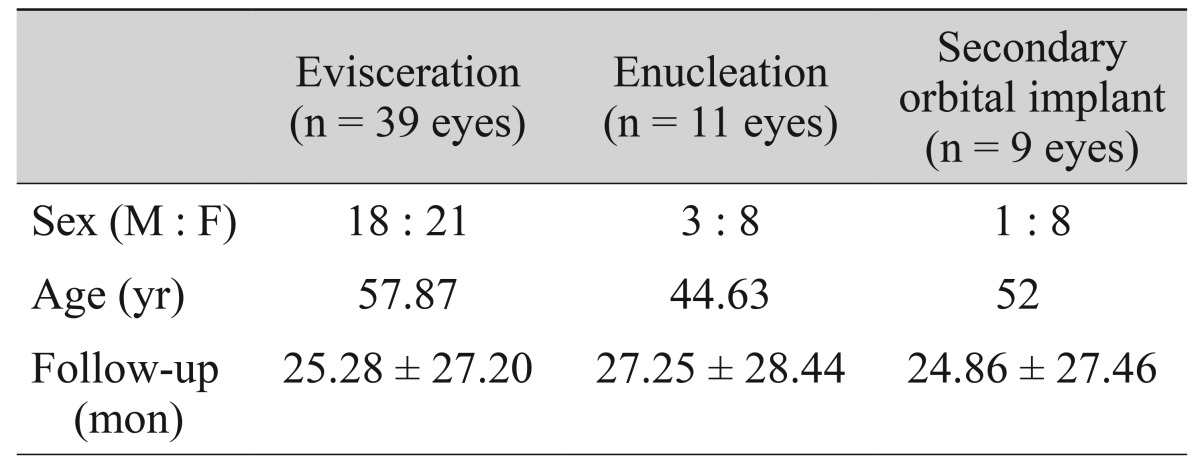
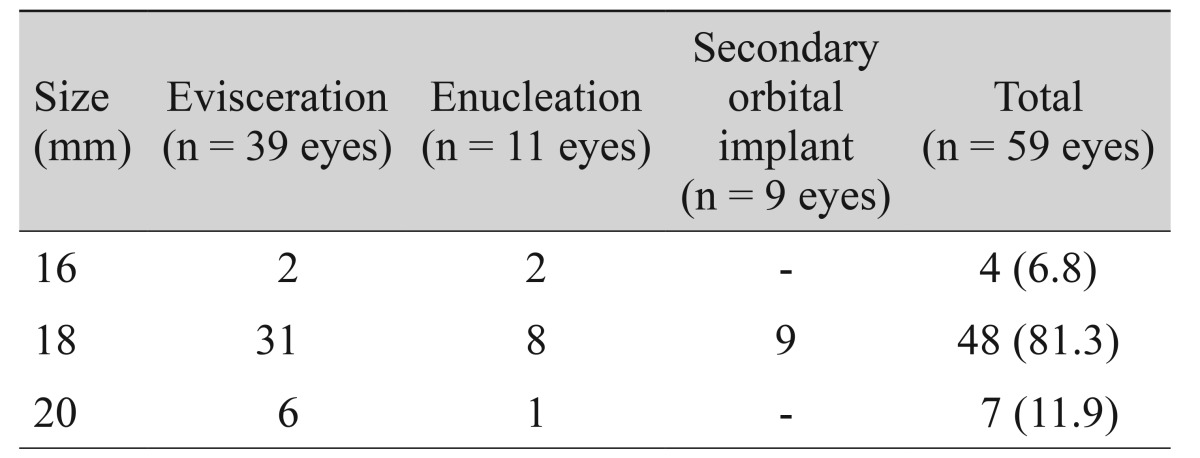
Surgery with the use of an MCOI was performed on 59 eyes. Evisceration was performed in 39 eyes (66.1% of total eyes), enucleation was performed in 11 eyes (16.6%), and secondary enucleation was performed in nine eyes (15.3%). The mean duration of follow-up care was 24.86 months (range, 6 to 90 months), with 25.28 ± 27.20 months for evisceration follow up, 27.25 ± 28.44 months for enucleation follow up, and 24.86 ± 27.46 months for secondary enucleation follow up (Table 1).
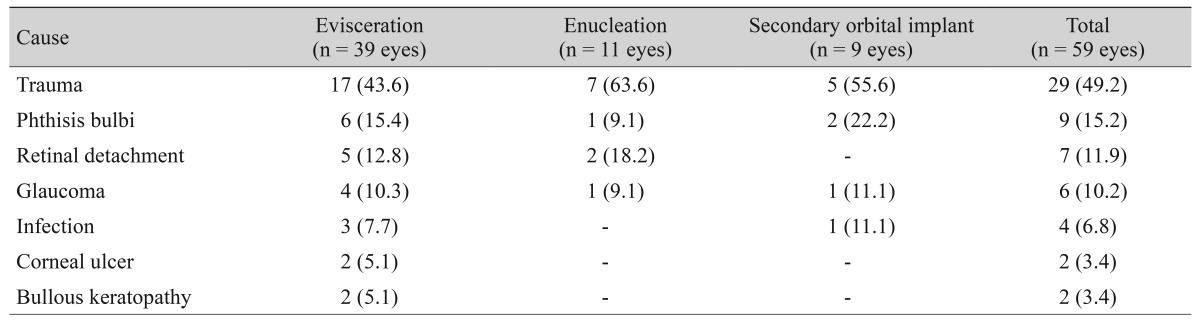
Trauma was the most frequent cause in cases requiring evisceration, enucleation, and secondary enucleation in a total of 29 eyes (49.2%). For evisceration alone, trauma was again the most frequent cause (43.6%), followed by phthisis bulbi (15.4%), chronic retinal detachment (12.8%), and glaucoma (10.3%). Trauma was also the most frequent cause in cases requiring enucleation (63.6%) and secondary enucleation (55.6%) (Table 2).
The orbital implant size was determined using a sizing ball during surgery, and an appropriately-sized orbital implant was inserted into the eye sockets of the patients. One of three orbital implant sizes of 16, 18, or 20 mm was selected for each eye, as appropriate. The 16-mm implant was used for four eyes (6.8%), the 18-mm implant was used for 48 eyes (81.3%), and the 20-mm implant was used for seven eyes (11.9%) (Table 3). Although the 18-mm implant was used most frequently (81.3%), four eyes received a 16-mm orbital implant due to small conal volume. Any orbital implant has to replace the maximum amount of lost orbital volume while avoiding implant exposure, thus making the selection of an appropriate orbital implant size critically important.
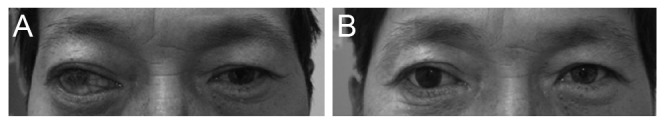
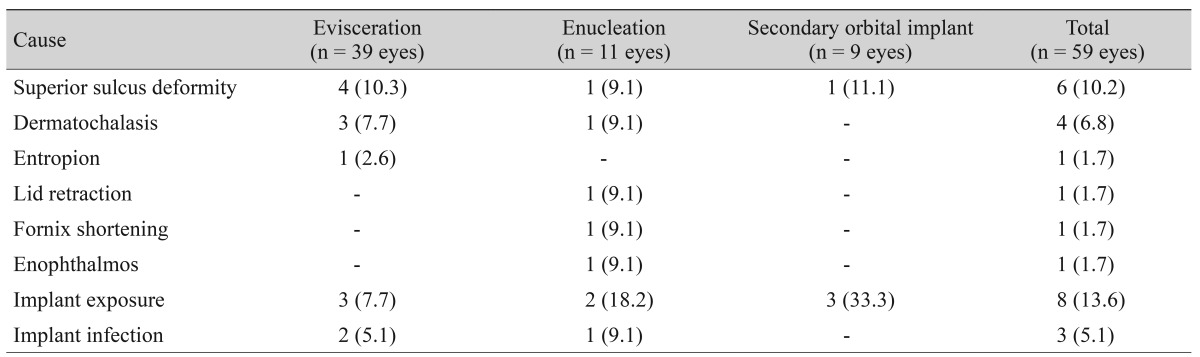
Among the 59 eyes, 41 eyes (69.4%) were of satisfactory postoperative cosmetic appearance (Fig. 2). Eighteen eyes developed postoperative complications, including orbital implant exposure in eight eyes (13.6%), superior sulcus deformity in six eyes (10.2%), and upper eyelid dermatochalasis in four eyes (6.8%). Ten eyes received secondary surgical interventions to correct complications. Of these ten eyes, six eyes (10.1%) with orbital implant exposure underwent reconstruction using an oral mucosa or dermal fat graft. In the remaining four eyes (6.8%) with lid deformity, a superior sulcus deformity correction or blepharoplasty was performed in two eyes and two eyes (3.4% and 3.4%), respectively (Table 4).
Orbital implant exposure was the most frequent postoperative complication. This occurred in eight eyes (13.6%), six of which received additional surgical reconstruction using an oral mucosa or dermal fat graft. In the orbital implant exposure group, the preoperative status of the Tenon's capsule and conjunctiva preservation were poor in all of the cases. Three eyes underwent secondary enucleation because of previous orbital implant exposure. One eye had been operated on because of traumatic eyeball rupture. Another one eye had a history of corneal ulceration, and had been operated on previously. Orbital implant infection occurred in three eyes, all of which were accompanied by orbital implant exposure. The second most frequent postoperative complication was superior sulcus deformity, found in six eyes (10.2%), two of which received surgical correction. Upper eyelid dermatochalasis was reported in four eyes (6.8%), two of which underwent blepharoplasty. Other complications included retraction of the upper eyelid, shortening of the inferior fornix, and lid ectropion, each respectively occurring in one eye (1.7%) (Table 4).
A 16-mm orbital implant was used in four eyes because of an inherently small orbital volume. One eye (25%) developed superior sulcus deepening, which was corrected by additional surgical intervention.
There have been numerous efforts to improve the shape and composition of orbital implants for ophthalmology patients in procedures of evisceration, enucleation, and secondary enucleation. An ideal orbital implant must replace the lost orbital volume, enhance motility, maintain symmetry, and have a good cosmetic appearance postoperatively. Moreover, the implant must be easily inserted, remain in a stable condition, and promote appropriate wound healing. The numerous aspects that must be taken into account make it difficult to choose an appropriate implant.
Insufficient wound closure can lead to wound dehiscence and infection [6,7,8]. Orbital implant exposure can occur when inserting an oversized orbital implant to replace the lost conal space, on applying an orbital implant without considering the shape of the orbital space, and when implanting an artificial eye before sufficient wound healing has occurred [6,9,10]. In contrast, using a too-small orbital implant to prevent orbital implant exposure can lead to poor cosmetic outcomes, including superior sulcus deepening, and implant migration because of insufficient volume replacement.
Orbital volume deficiency after replacement with an orbital implant in evisceration and enucleation is a frequent postoperative complication. The risk may increase with not only the use of a small orbital implant, but also when the lost orbital space is not sufficiently replaced. Insufficient orbital volume replacement can lead to the inferior and posterior displacement of the superior rectus-levator complex, causing superior sulcus deformity and backward tilting of the implant [11]. Ultimately, these conditions can result in retraction of the preaponeurotic fat pad, shortening of the inferior fornix, and facial asymmetry. The work of Kaltreider et al. [12] reports that 70% to 80% of the orbital volume removed from an eye must be replaced to avoid volume deficiency. However, closure of the sclera over the implant after removal of the cornea and anterior chamber consequently cause anterior orbital volume loss, which cannot be easily replaced. The anatomical shape of the orbital space is conical, which makes it difficult for traditional orbital implants (which are spherical) to sufficiently replace the lost orbital volume. Furthermore, using an overly large orbital implant in replacing the space may lead to fornix narrowing and an increased rate of implant exposure [2].
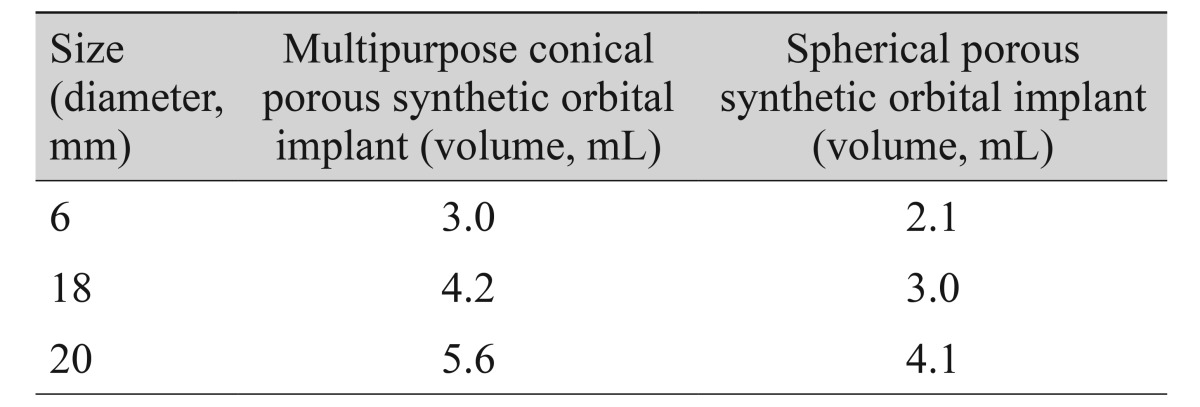
The MCOI (Medpor) more closely matches the natural anatomical shape of the orbit relative to traditional spherical orbital implants (Fig. 1). A posterior portion of the MCOI, which projects to the conal apex and is parallel to the orbital wall, provides additional volume for the conal apex. The portion is 2 mm longer than a spherical orbital implant of the same size, and can more effectively replace the orbital volume. This longer posterior portion provides greater conal apex volume, and thus prevents enophthalmos, superior sulcus deformity, and orbital implant migration. Furthermore, its conical shape minimizes disruption of the extraocular muscle movement in the conal space. The anterior portion of the implant has a broader and more flattened design, thus providing the advantage of replacing lost anterior volume, while also replacing anterior orbital volume and preventing anterior tilting of the inferior rectus muscle due to the vertically longer and broader anterior area. Furthermore, the round anterior area of the implant offers the added advantage of dispersing the pressure while closing the anterior orbital area. Conjunctival closure can be easily performed, while minimizing tension in the Tenon's capsule after closure. The design of the implant also minimizes the development of a focal pressure point between the implant and prosthesis, thus potentially preventing erosion of the conjunctiva [2]. The specific design of the MCOI has a greater volume in comparison to a spherical orbital implant of the same size. According to product descriptions of the Medpor, the 16-mm MCOI has a volume of approximately 3 mL in comparison to 2.1 mL for the spherical implant, while the 18-mm MCOI has a volume of 4.2 mL in comparison to only 3 mL for its spherical counterpart (Table 5). With this additional volume, the MCOI can sufficiently replace the lost orbital volume in common orbital implant procedures.
Although a spherical implant offers symmetry and is similar in shape to the eyeball, it has inherent disadvantages. In orbital implant surgery, fibrovascular ingrowth is a major indicator of success [5]. An increased surface area may promote fibrovascular ingrowth within an orbital implant. Compared to a spherical shape, the conical shape has a larger surface area, thereby potentially increasing the success rate of the implant.
The MCOI is composed of porous polyethylene, which is readily molded from high-density polyethylene powder. This material is nonallergenic, nontoxic, and biocompatible [13]. It allows fibrovascular proliferation and reduces the risk of orbital implant migration, exposure, and extrusion, while minimizing the rate of infection. The material is not brittle, which allows the direct suturing of rectus muscles to the implant without the need for other wrapping materials [3,14,15,16,17]. Regarding surgical techniques, the material is able to simplify complicated surgical procedures to such an extent that it is usefully applied in various types of anophthalmic orbital-implant surgeries.
Generally speaking, orbital implant exposure is one of the major postoperative complications in orbital implant surgery. In the present study, orbital implant exposure was the most frequent complication, found in eight of 59 eyes (13.6%). Exposure rates in the existing literature vary from 0% to 21% [13]. The work of Alwitry et al. [13] investigates the spherical Medpor, which is manufactured from the same porous polyethylene material, but is spherical in shape rather than conical. The research reports implant exposure in 14 of 106 eyes (13.2%). The work of Baek [18] reports a 13.7% exposure rate using a porous polyethylene orbital implant, which is a similar percentage to our outcomes.
In the present study, superior sulcus deformity occurred in six of the eyes receiving the MCOI (10.2%), two of which received additional surgical corrections to improve the postoperative cosmetic appearance (3.4%). The work of Marshak and Dresner [2] reports no superior sulcus deformities in 30 eyes that received evisceration using the MCOI. A study by Rubin et al. [5] reports a moderate rate of superior sulcus deformity in two of 43 eyes (4.65%) when grading the degree of superior sulcus deformities as mild, moderate, or severe in enucleation using the MCOI, thus suggesting that the MCOI has an advantage with regard to superior sulcus deformities. Similarly, in the present study, only two eyes required additional surgery to correct postoperative superior sulcus deformities.
Blepharoptosis was found in four eyes (6.8%), two of which received upper eyelid blepharoplasty (3.4%). The work of Shoamanesh et al. [19] reports a 19.74% blepharoptosis rate, together with a 4.98% surgical correction rate in a group of patients undergoing surgery using traditional spherical synthetic porous polyethylene orbital implants. In the present study, the blepharoptosis incidence was lower with the MCOI. The study by Shoamanesh et al. [19] reports a rate of 15.7% for fornix insufficiency. The present study, however, finds fornix shortening in only one eye (1.7%) (Table 4).
A 16-mm MCOI was inserted in four eyes with inherently small orbital volumes. Using an 18-mm MCOI in eyes with a small volume may increase the risk of excessive tension, whereas the traditional 16-mm spherical orbital implant may increase the risk of insufficient volume replacement. The volume of a 16-mm spherical implant is 2.1 mL, whereas the volume of the conical implant is approximately 3 mL. Therefore, the conical orbital implant provides a greater volume than a spherical implant of the same size, and thus more effectively replaces the lost orbital volume without causing excessive tension. One eye required additional corrective surgery for upper eyelid deformity (25%), whereas the other three eyes showed no postoperative complications.
Relative to the traditional spherical orbital implant, the conical orbital implant may have the advantages of preventing upper eyelid deformity with sufficient volume replacement and reducing implant exposure by minimizing tension. Consequently, the reported rates of blepharoptosis and fornix insufficiency in the present study were lower for the conical orbital implant than in existing literature about implant surgeries using traditional spherical orbital implants. On the other hand, the implant exposure rates were similar between conical and traditional implants. However, previous literature has focused on the complications related to implant exposure, whereas morphologic changes of eyelids have rarely been studied. This provides certain challenges when specifically comparing morphologic complications of eyelids. In addition, comparisons between spherical and conical implants used in implant surgeries by the same surgeon have not been conducted, and therefore, future studies should reflect this limitation.
Anophthalmic socket surgery has been used for many years to control pain and orbital infection. Only functional complications, including implant exposure, have received particular attention in the research. However, cosmetic problems are of increasing importance for patients who have undergone implant surgery. Therefore, further studies with a larger population and longer follow-up period are required for investigating cosmetic problems among orbital implant surgery patients.
The present study reports the clinical outcomes of various orbital implant surgeries conducted with the MCOI, which to date has not been greatly investigated in existing research. The MCOI may minimize cosmetic and morphologic complications in patients relative to spherical implants. Moreover, the results emphasize the need to consider cosmetic outcomes when performing anophthalmic socket surgery using an orbital implant.
Notes
The results of this study were presented at the 112th annual meeting of the Korean Ophthalmological Society.
Conflicts of interest
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Smit TJ, Koornneef L, Zonneveld FW, et al. Computed tomography in the assessment of the postenucleation socket syndrome. Ophthalmology 1990;97:1347-1351.


2. Marshak H, Dresner SC. Multipurpose conical orbital implant in evisceration. Ophthal Plast Reconstr Surg 2005;21:376-378.


3. Hornblass A, Biesman BS, Eviatar JA. Current techniques of enucleation: a survey of 5,439 intraorbital implants and a review of the literature. Ophthal Plast Reconstr Surg 1995;11:77-86.


4. Lee JH, Cho WC. A case of Medpor orbital implant infection. J Korean Ophthalmol Soc 2001;42:783-787.
5. Rubin PA, Popham J, Rumelt S, et al. Enhancement of the cosmetic and functional outcome of enucleation with the conical orbital implant. Ophthalmology 1998;105:919-925.


6. Chalasani R, Poole-Warren L, Conway RM, Ben-Nissan B. Porous orbital implants in enucleation: a systematic review. Surv Ophthalmol 2007;52:145-155.


8. Jordan DR, Gilberg S, Bawazeer A. Coralline hydroxyapatite orbital implant (bio-eye): experience with 158 patients. Ophthal Plast Reconstr Surg 2004;20:69-74.


9. Blaydon SM, Shepler TR, Neuhaus RW, et al. The porous polyethylene (Medpor) spherical orbital implant: a retrospective study of 136 cases. Ophthal Plast Reconstr Surg 2003;19:364-371.


10. Colen TP, Paridaens DA, Lemij HG, et al. Comparison of artificial eye amplitudes with acrylic and hydroxyapatite spherical enucleation implants. Ophthalmology 2000;107:1889-1894.


11. Kronish JW, Gonnering RS, Dortzbach RK, et al. The pathophysiology of the anophthalmic socket. Part II. Analysis of orbital fat. Ophthal Plast Reconstr Surg 1990;6:88-95.


12. Kaltreider SA, Jacobs JL, Hughes MO. Predicting the ideal implant size before enucleation. Ophthal Plast Reconstr Surg 1999;15:37-43.


13. Alwitry A, West S, King J, et al. Long-term follow-up of porous polyethylene spherical implants after enucleation and evisceration. Ophthal Plast Reconstr Surg 2007;23:11-15.


14. Jung SK, Cho WK, Paik JS, Yang SW. Long-term surgical outcomes of porous polyethylene orbital implants: a review of 314 cases. Br J Ophthalmol 2012;96:494-498.


15. Lee S, Maronian N, Most SP, et al. Porous high-density polyethylene for orbital reconstruction. Arch Otolaryngol Head Neck Surg 2005;131:446-450.


16. Klawitter JJ, Bagwell JG, Weinstein AM, Sauer BW. An evaluation of bone growth into porous high density polyethylene. J Biomed Mater Res 1976;10:311-323.


17. Spector M, Flemming WR, Sauer BW. Early tissue infiltrate in porous polyethylene implants into bone: a scanning electron microscope study. J Biomed Mater Res 1975;9:537-542.


18. Baek SH. Clinical effect of porous polyethylene (Medpor(r)) orbital implant. J Korean Ophthalmol Soc 2000;41:1858-1863.
Fig. 1
(A) Schematic image of a multipurpose conical porous synthetic orbital implant (MCOI; Medpor, Porex Surgical, College Park, GA, USA). Posterior projection parallel to the orbital walls. The front end is flattened and widened. (B) Sagittal view of the MCOI in magnetic resonance imaging. (C) Conal-shaped MCOI.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




