Aflibercept Treatment for Neovascular Age-related Macular Degeneration and Polypoidal Choroidal Vasculopathy Refractory to Anti-vascular Endothelial Growth Factor
Article information
Abstract
Purpose
To report the results of switching treatment to vascular endothelial growth factor (VEGF) Trap-Eye (aflibercept) in neovascular age-related macular degeneration (AMD) and polypoidal choroidal vasculopathy (PCV) refractory to anti-VEGF (ranibizumab and bevacizumab).
Methods
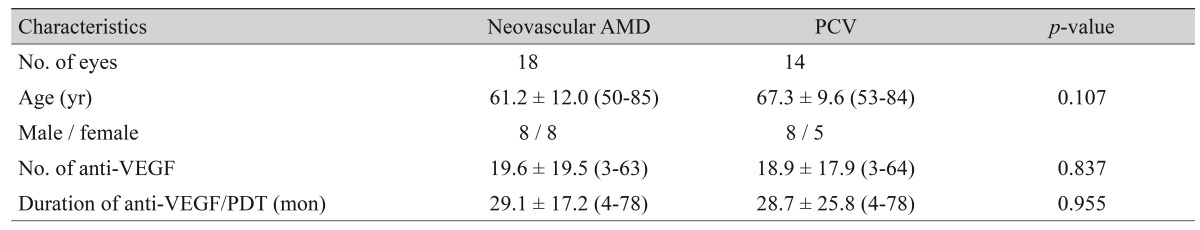
This is a retrospective study involving 32 eyes from 29 patients; 18 were cases of neovascular AMD and 14 were cases of PCV. The best-corrected visual acuity (BCVA) and central macular thickness (CMT) of spectral-domain optical coherence tomography were evaluated.
Results
BCVA and CMT improved from 0.58 to 0.55 (p = 0.005) and from 404 to 321 µm (p < 0.001), respectively, after switching to aflibercept. The 14 eyes that received 6 or more aflibercept injections remained stable at 0.81 to 0.81 and 321 to 327 µm (p = 1.0, 0.29), respectively, after 3 aflibercept injections. The 10 eyes that received 3 or more bevacizumab injections after 3 or more aflibercept injections worsened, from 0.44 to 0.47 and from 332 to 346 µm (p = 0.06, 0.05), respectively. The results showed similar improvement of BCVA and CMT in neovascular AMD and PCV.
Conclusions
Aflibercept seems to be effective for improvement and maintenance of BCVA and CMT for neovascular AMD and PCV refractory to anti-VEGF. Switching from aflibercept back to bevacizumab treatment may not be a proper strategy.
Neovascular age-related macular degeneration (AMD) is a leading cause of blindness in aged populations in the industrialized world [123]. Currently, intravitreal injection of anti-vascular endothelial growth factor (VEGF) is the standard therapy for treating neovascular AMD [45]. Bevacizumab and ranibizumab injections play important roles in preserving vision and preventing vision loss [678]. However, for approximately 10% of AMD cases, treatment with anti-VEGF has been reported to have no initial effect or induce resistance with repeated treatments [910]. Possible mechanisms of resistance are tolerance or tachyphylaxis, which is defined as decreased response to repeated treatment with a medication [1011].
Polypoidal choroidal vasculopathy (PCV) is characterized by frequent recurrence, bilateral asymmetry, and serous and hemorrhagic detachment of retinal pigment epithelium, which can also cause vision loss [12]. Among several treatment strategies, photodynamic therapy (PDT) and intravitreal injection of anti-VEGF have shown the most favorable results [1314]. However, serious complications such as foveal atrophy after PDT and limited responsiveness to anti-VEGF treatment have also been reported [1415].
Possible countermeasures include temporary cessation [10] or increasing the volume of anti-VEGF [16]. However, these measures might result in deterioration of the lesions or increase the risk of adverse effects. Another possible countermeasure is the introduction of a drug with a different mode of action [10]. In this context, aflibercept, which has a different mode of action compared to anti-VEGF, is expected to be a novel treatment option for the above cases by acting as a 'trap system' [1718].
In this study, we evaluated the visual and anatomical response of intravitreal injection of aflibercept in eyes with neovascular AMD and PCV refractory to treatment with ranibizumab or bevecizumab.
Materials and Methods
Design
This study is a retrospective chart review of patients with neovascular AMD and PCV refractory to treatment with ranibizumab or bevecizumab. They were switched to aflibercept treatment with at least 3 consecutive injections at approximately one-month intervals between July 1, 2013 and June 30, 2014.
Patient selection
Inclusion criteria of this study are as follows: known choroidal neovascularization secondary to AMD or PCV diagnosed with fluorescein angiography and indocyanine green angiography, persistent or recurrent fluids on spectral-domain optical coherence tomography (SD-OCT), or leakage on angiography after 3 or more anti-VEGF treatments prior to switching to aflibercept. After switching, patients with more than three initial monthly loading doses of intravitreal aflibercept (2 mg in 0.05 mL) were enrolled.
Follow-up examination and data
A full ophthalmic examination, including best-corrected visual acuity (BCVA), intraocular pressure, slit lamp examination, indirect ophthalmoscopy, fundus photograph, and SD-OCT (Heidelberg Spectralis; Heidelberg Engineering, Heidelberg, Germany) were conducted at each monthly visit. Demographic data and treatment history (number of injections and duration of follow-up) were also collected. BCVA (Snellen) were obtained on the day of aflibercept initiation, at subsequent follow-up visits, and at the final follow-up visit. Central macular thickness (CMT) was calculated with custom software. Segmentation lines and central foveal location were manually adjusted when necessary.
Analysis
The primary outcomes of this study were the mean change in logarithm of the minimal angle of resolution in visual acuity and CMT after switching to aflibercept injections. SD-OCT was used to analyze the fluid resolution including the intraretinal fluid, subretinal fluid, pigment epithelial detachments, and subretinal hemorrhage. Changes of the fluid from baseline were classified as complete resolution, partial resolution, unchanged or worse. Complete resolution was defined as resolution of all components of the fluid from baseline. The same analysis was conducted in each of the neovasuclar AMD (18 cases) and PCV (14 cases) patients. Further analysis was performed in patients treated with aflibercept 3 to 4 times and more than 4 times (aflibercept on-going) as well as on those who returned to bevacizumab treatment with more than 3 injections (switching-back). Statistical analysis was performed using the SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). Wilcoxon signed rank tests were used to compare the differences in means between baseline and follow-up examinations for BCVA and CMT. Mann-Whitney U-tests were used to identify the differences in baseline characteristics between AMD and PCV patients. A p-value less than 0.05 was considered to be statistically significant.
Results
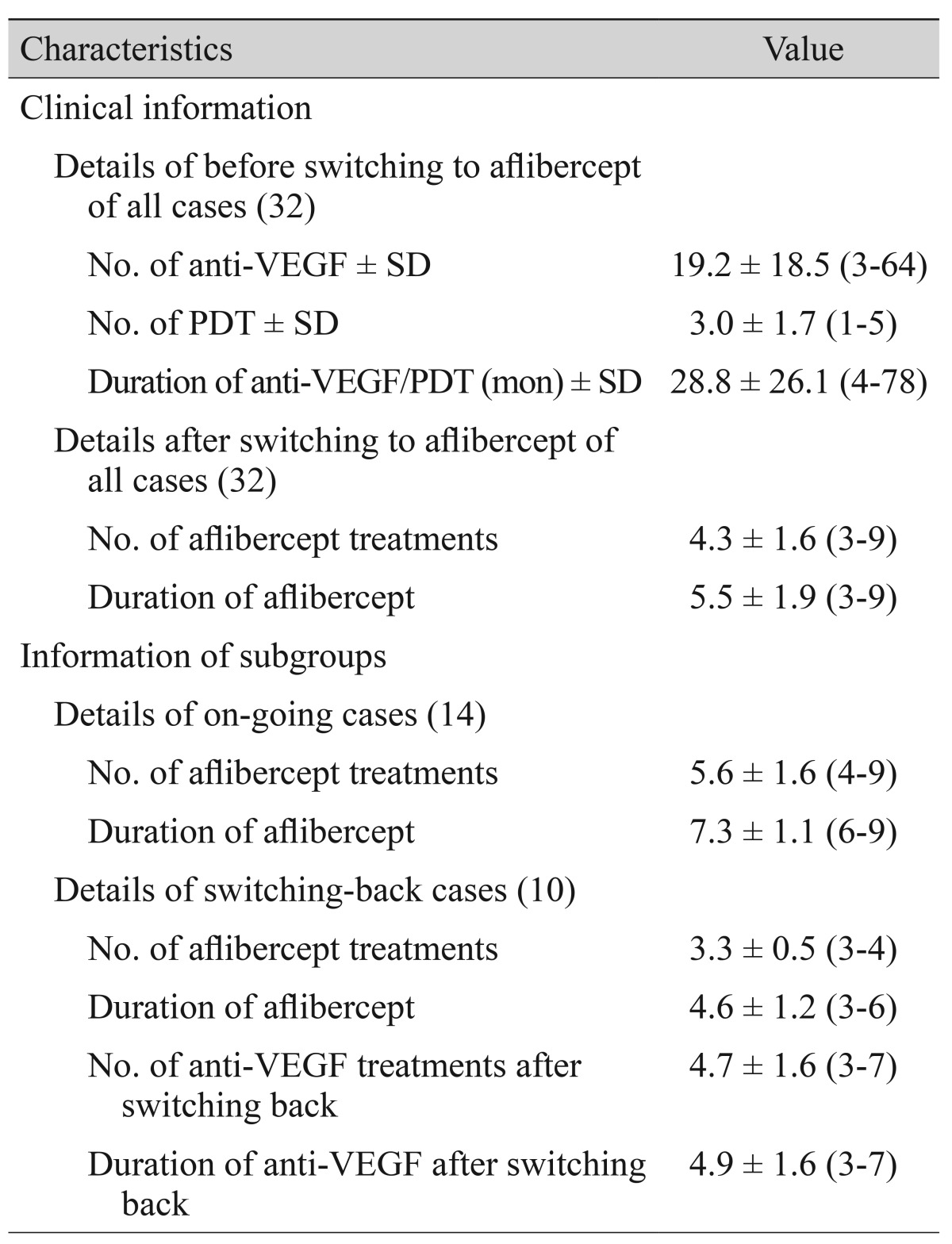
patient characteristics at the time of switching to aflibercept (baseline) for 32 cases (17 refractory cases, 15 recurrent cases) of 29 pateints (16 male and 13 female) are listed in Table 1. The mean age at baseline was 63.8 ± 11.3 years (range, 50 to 85 years). The clinical characteristics of all cases are listed in Table 2. All cases were treated three or more times with other drugs before switching to aflibercept: 12 were previously treated with bevacizumab alone, 7 with ranbizumab, 13 with both bevacizumab and ranibizumab, and 10 were treated with PDT on one or more occasions. The mean number and duration of anti-VEGF/PDT treatment prior to switching were 19.2 times (range, 3 to 64 times) / 3.0 (1 to 5) and 28.8 months (range, 4 to 78 months), respectively. The mean number and duration of aflibercept injection after switching were 4.3 times (range, 3 to 9 titmes) and 5.5 ± 1.9 months (range, 3 to 9 months), respectively. Out of all cases, 8 were treated with only 3 to 4 aflibercept injections (loading treatment), 14 were treated with more than 4 aflibercept injections and 6 month follow-up (on-going treatment) because of excellent clinical response to aflibercept or patient requests. There were 10 cases treated with bevacizumab again (switching-back treatment) after 3 or 4 injections of aflibercept due to poor response to aflibercept or expense issues despite excellent response to aflibercept.
Changes in mean BCVA were measured (Fig. 1). BCVA significantly improved at all follow-up visits compared with baseline (p = 0.005). The mean BCVA improvement was highest at 2.7 months after switching to aflibercept (p = 0.003). The mean BCVA improved from 0.31 to 0.24 (p = 0.06) in the loading treatment patients (8 eyes) and remained stable, changing from 0.81 to 0.81 (p = 1.0), in the on-going treatment patient group (14 cases) who were injected with aflibercept 4 or more times and received continual follow-up for 6 months. The average number of additional aflibercept injections and follow-up were 2.6 times and 3.1 months, respectively. However, the mean BCVA deteriorated from 0.44 to 0.47 (p = 0.06) in the switching-back treatment patient group (10 cases) who were returned to bevacizumab injections administered an average of 4.7 times (range, 3 to 7 times) over 4.9 months (range, 3 to 7 months).
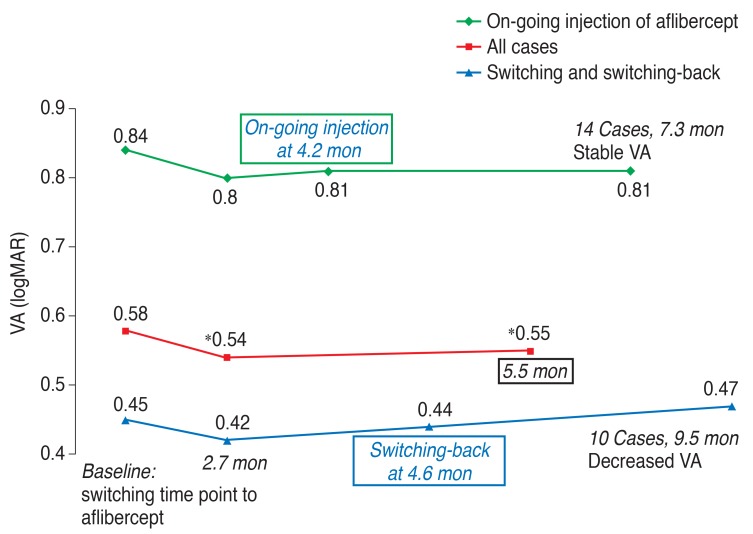
Changes in mean best-corrected visual acuity (logarithm of the minimal angle of resolution, logMAR) for all cases including on-going and switching-back cases during the entire follow-up period. 2.7 months was the time point after 3 initial loading injections of aflibercept in all cases. 4.2 months was the time point of 4 or more on-going treatment of aflibercept in 14 cases. 4.6 months was the time point of switching-back treatment of bevacizumab in 10 cases. Improvement of best-correct visual acuity from baseline of all cases was statistically significant, but not significant in on-going or switching-back treatment cases during the entire follow-up period. Best-correct visual acuity was stable in on-going cases (p = 1.0) but deteriorated in switching-back cases (p = 0.06). VA = visual acuity. *p < 0.05.
There was no significant difference in the change in the mean BCVA between the two patient groups (on-going and switching-back) from baseline to final follow-up period (p = 0.102 and 0.414, respectively). However, the BCVA worsened by more than 1 line from the baseline in 4 of the switching-back patients, whereas there was no worsening in the on-going group. Demographic characteristics including BCVA, age, treatment history (anti-VEGF and PDT), and duration of disease did not show significant differences between the on-going and switching-back treatment patients (data not shown).
Anatomical changes were analyzed for all groups (Fig. 2). CMT reduction changed significantly for all follow-up visits compared with baseline measurements (p = 0.000). The maximum mean reduction was 83 µm at 4.6 months, which corresponded to the time point just before switching back to bevacizumab in 10 of the 32 cases. Similar to the visual acuity changes, CMT improved from 341 to 291 µm (p = 0.04) in loading treatment patients (8 eyes) and remained stable in the on-going treatment patient group (14 cases) during the treatment period (321 to 327 µm, p = 0.29). Meanwhile, CMT deteriorated in the switching-back treatment patient group (10 cases) during the switch-back period (332 to 346 µm, p = 0.05). The mean change in CMT was statistically significant only in the on-going treatment patients (14 cases, p = 0.02) from baseline to the final follow-up period.

Changes in mean central macular thickness (CMT) of all cases, on-going cases, and switching-back cases during the entire follow-up period. 4.2 months was the time point of 4 or more on-going treatments of aflibercept in 14 cases. 4.6 months was the time point of switching-back treatment of bevacizumab in 10 cases. Improvement of CMT from baseline in all cases, including on-going and switching-back cases, was statistically significant during the entire follow-up period. However, after switching back to bevacizumab, CMT increased (p = 0.05) during the switching-back period. In contrast, CMT remained stable in on-going 4 or more treatment cases of aflibercept (p = 0.29) during the treatment period. *p < 0.05.
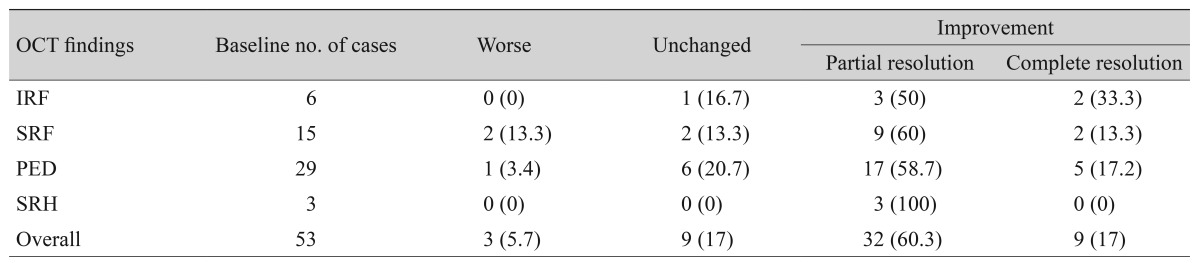
Further analyses for SD-OCT were also conducted (Table 3) [5]. Upon qualitative analysis of OCT findings [5], 6 cases with intraretinal fluid, 15 with subretinal fluid, 29 with pigment epithelial detachment, and 3 with subretinal hemorrhage were observed at the baseline. After switching to aflibercept, more than 70% of patients responded to treatment. However, 17% were unchanged and 6% had a worsening of their condition.
Subanalysis of SD-OCT findings in the on-going and switching-back groups showed maintenance of the results in 91.6% (11 / 12) of the on-going group. In the switching-back group, the SD-OCT results worsened in 35.3% (7 / 16) of cases and was maintained in 64.7% (11 / 17) (data not shown).
Another analysis of the changes in SD-OCT findings, CMT and BCVA of choroidal neovascularization (18 cases), and PCV (14 cases) patients showed similar results: overall treatment response was more than 70% in both patient groups, BCVA and CMT improved respectively from 0.54 to 0.51 (p = 0.06) and 409 to 341 (p = 0.017) in neovascular AMD and from 0.64 to 0.61 (p = 0.06) and 398 to 308 (p = 0.005) in PCV (data not shown).
Adverse events
No ocular adverse events were observed, including endophthalmitis, retinal detachment, retinal pigment epithelial tears, submacular hemorrhage, uveitis, or sustained intraocular pressure elevation requiring other treatment.
Discussion
It has been reported that aflibercept is an effective treatment not only for patients with naïve neovascular AMD [19] but also for those who show no response or resistance to existing anti-VEGF treatments [452021]. In this study, switching to aflibercept resulted in significant improvement in visual acuity and CMT in AMD and PCV patients who showed no response or resistance to existing treatments. In addition, improved visual acuity and CMT were maintained for more than 6 months in the group that continued aflibercept treatment.
Notably, we analyzed the results of switching-back treatment, which involves returning to anti-VEGF treatment after switching to aflibercept. Unlike the results of the on-going treatment, there was deterioration in visual acuity and CMT in the 10 patients who were switched back to bevacizumab. The reason for switching back to bevacizumab was cost for 5 cases, even though they were responsive to aflibercept. The other 5 cases were not responsive to aflibercept. Although the numbers of cases were small, these data suggest that switching back from aflibercept to bevavizumab is not an effective strategy.
These data might be derived from the differences in the basic affinity of each drug for receptors. Aflibercept, which is a trap-eye system and works on placental growth factor as well as VEGF B, has better affinity to VEGF A than existing anti-VEFG drugs such as ranibizumab and bevacizumab, which are anti-VEFG antibodies [1718]. In addition to potency, abrupt discontinuation of aflibercept may be another explanation. For uveitis, changes into less potent drugs deteriorated the disease progress. Thus, slow tapering of the drug may be more effective for these cases. This observation also suggests that switching back to bevacizumab after gradual discontinuation of aflibercept using methods such as the treat and extend or capped pro re nata in the VEGF-Trap Eye: Investigation of Efficacy and Safety in Wet AMD (VIEW) study are possible solutions when switching treatment from aflibercept back to bevacizumab is inevitable [19]. Another possible solution is switching back to super-high or high dose anti-VEGF treatment. The SAVE (Super-dose Anti-VEGF) study already demonstrated the effectiveness of super-high dose anti-VEFG treatment for recalcitrant neovascular AMD [16]. Since the cost difference between aflibercept and bevacizumab may result in more switching-back treatments, further long-term studies on gradual discontinuation are needed. Additionally, identification of deteriorating factors in switching back as well as baseline patient demographic characteristics are required. Studies on switching to ranibizumab and switching from naïve aflibercept treatment are also needed.
In this study, 9 patients did not show appropriate responses to aflibercept. When the cases were divided into responsive and non-responsive groups, significant differences (p = 0.018, Mann-Whitney test) in the duration of disease were observed between the groups. The area under the receiver operating characteristic curve was 0.77 (p = 0.019), implying that long-duration of disease led to less effective aflibercept treatment (in refractory cases).
Limitations of this study include retrospective chart review, low case number, short-term follow-up, and non-controlled study. However, this study was not designed to test a hypothesis but to identify a trend in the management of refractory AMD and PCV cases. Thus, further prospective and controlled studies with higher case numbers and long-term follow-up are needed.
In conclusion, switching treatment to aflibercept seems to be effective for improvement and maintenance of BCVA and CMT over 6months for neovascular AMD and PCV refractory to anti-VEGF. In addition, switching back to bevacizumab is not recommended and further study of switching back the treatment to prior anti-VEGF is necessary.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.