Massive Exudative Retinal Detachment Following Photodynamic Therapy and Intravitreal Bevacizumab Injection in Retinal Capillary Hemangioma
Article information
Dear Editor,
Retinal capillary hemangioma (RCH) is a benign capillary angiomatous hamartoma that occurs on the peripheral or juxtapapillary retina. The condition in which RCH is accompanied by intracranial hemangioblastomas and cysts in abdominal organs such as kidneys or pancreas is termed von Hippel-Lindau (VHL) disease. Photodynamic therapy (PDT) with anti-vascular endothelial growth factor agents is an effective treatment for RCH [1], although exudative complications can occur following PDT in rare cases [2,3,4]. Herein, we present a case of massive exudative retinal detachment involving the entire retina following the administration of PDT with intravitreal injection of bevacizumab in a patient with VHL disease.
A 24-year-old man was referred to our hospital with a history of impaired vision in his left eye. On admission, his visual acuity was 20 / 100 in the left eye, and his medical history revealed a previous diagnosis of VHL disease with multiple cerebellar hemangioblastomas and renal cell carcinoma. Furthermore, the patient had a family history of VHL disease, and genetic analyses revealed a mutation in the VHL tumor suppressor gene (VHL gene). Two months prior to the development of visual symptoms, he had undergone suboccipital craniectomy and excision of the cerebellar hemangioblastomas. Fundus examination revealed an inferonasal, 2-disc diameter-sized RCH with dilated feeder vessels (Fig. 1A). The patient was recommended PDT, which he declined.
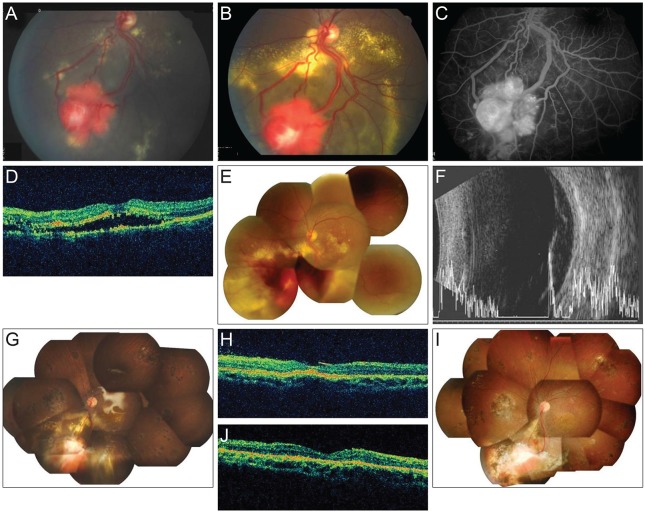
Fundus photographs of the left eye of our 24-year-old patient with confirmed von Hippel-Lindau disease obtained at the initial visit (A) and two years later (B). A peripheral retinal capillary hemangioma with dilated feeder vessels was observed. A fundus fluorescence angiography image (C) revealed leakage from the hemangioma, and optical coherence tomography (OCT) showed shallow subretinal fluid (D). Fourteen days after photodynamic therapy combined with an intravitreal injection of bevacizumab, fundus photography (E) and ultrasonography (F) revealed massive exudative retinal detachment with retinal hemorrhage. Two months after pars plana vitrectomy with silicone oil tamponade, fundus photography (G) and OCT (H) showed that the retina had reattached, and the subretinal fluid had disappeared. One year after silicone oil removal, fundus photography (I) and OCT (J) showed no retinal capillary hemangioma recurrence or subretinal exudation.
Two years later, the patient revisited our clinic with a complaint of double vision. The visual acuity in his left eye was 20 / 1,000, and fundus examination revealed an enlarged RCH with exudation (Fig. 1B and 1C). Optical coherence tomography revealed subretinal fluid accumulation with macular involvement (Fig. 1D).
PDT with a 6 mg/m2 (body surface area) dose of verteporfin over a period of 10 minutes and a light exposure of 50 J/cm2 5 minutes after intravenous verteporfin injection were administered in combination with an intravitreal injection of 1.25 mg/0.05 mL bevacizumab (Avastin; Genentech-Roche, South San Francisco, CA, USA).
Fourteen days after PDT and intravitreal bevacizumab injection, the patient's visual acuity in the left eye progressed to no light perception. Funduscopy revealed total retinal detachment with massive exudation and hemorrhage from the RCH (Fig. 1E and 1F). After 21 days, his visual acuity showed no improvement, and total retinal detachment was still apparent. Consequently, we performed pars plana vitrectomy, internal subretinal fluid drainage retinotomy, endodiathermy, cryotherapy and endolaser therapy on the RCH, and injection of silicone oil and bevacizumab.
Two months after surgery, his visual acuity in the left eye recovered slightly to enable the detection of hand motion. Funduscopy revealed the absorption of subretinal fluid in the left eye (Fig. 1G and 1H). Six months after vitrectomy, the silicone oil was removed. One year later, the patient's visual acuity in the left eye had improved to 20 / 500 (Fig. 1I and 1J).
VHL disease is a dominantly inherited multi-systemic cancer syndrome associated with a mutation in the VHL gene. VHL protein dysfunction leads to upregulation of hypoxia inducible factors, which in turn leads to increased levels of angiogenic cytokines. Angiomatous proliferation is a target for RCHs and is aided by anti-angiogenic treatments. Furthermore, the treatment of RCH is variable and depends on the size, location, and secondary effects. Laser photocoagulation or cryotherapy is the standard treatment for small and medium-sized RCH. PDT for the treatment of peripheral RCH has shown effective results in terms of decreasing regional exudation from large lesions [1,5]. Furthermore, the complication of massive exudative retinal detachment after PDT is extremely rare; only two cases have been reported worldwide, one of which was managed by emergency vitrectomy [3,4]. The surgical outcomes of our case and the previous case [3] indicated successful removal of the subretinal fluid and restoration of vision. Unlike previous cases, we also administered an intravitreal injection of bevacizumab; however, this did not prevent massive exudation following PDT.
In summary, our case indicates that treatments for large RCHs in patients with VHL disease must be carefully selected. Although PDT is considered one of the useful treatment options for RCH, PDT combined with an intravitreal injection of bevacizumab can lead to permanent and severe deterioration of vision because of massive exudative retinal detachment. Therefore, frequent fundus examinations should be performed after PDT.
Acknowledgements
This study was supported by grant no. 14-2014-022 of the Seoul National University Bundang Hospital research fund.
Notes
No potential conflict of interest relevant to this article was reported.