Bilateral Macula-involving Metastatic Infection Resulting from Septic Embolization
Article information
Dear Editor,
Retinal features associated with septicemia usually do not involve the macula. However, there have been a small number of reports regarding macular hole cases secondary to septic emboli [1,2]. We report a case of bilateral macula-involving metastatic infection rather than macular hole resulting from septic embolization.
A 29-year-old man who had initially presented to the emergency room for altered mentality and been diagnosed with gram-positive cocci bacteremia and meningoencephalitis after work-up was referred for decreased bilateral vision, noted about 3 days after admission. Methicillin-sensitive Staphylococcus aureus was observed on blood culture. The patient began a 4-week course of intravenous penicillin G (4 million units every 4 hours). On initial examination, his best-corrected visual acuities (BCVA) were 20 / 40 in right eye and 20 / 100 in left eye. Fundus examination showed small white infiltration with hemorrhage in the juxtafovea of both eyes (Fig. 1A). Fluorescein angiography showed no active leakage (Fig. 1B). Spectral domain-optical coherence tomography images showed disruption at the junction of the photoreceptor inner and outer segments (IS/OS) junction and cone outer segment and hyperreflective intraretinal deposits involving both the inner and outer retinal layers at the fovea (Fig. 1C). The area of IS/OS junction and cone outer segment layer disruption was much wider and more extensive in the left eye, in which there was also a focal area of near total retinal tissue defect close to the shape of an impending macular hole in the juxtafovea of the left eye (Fig. 1D).
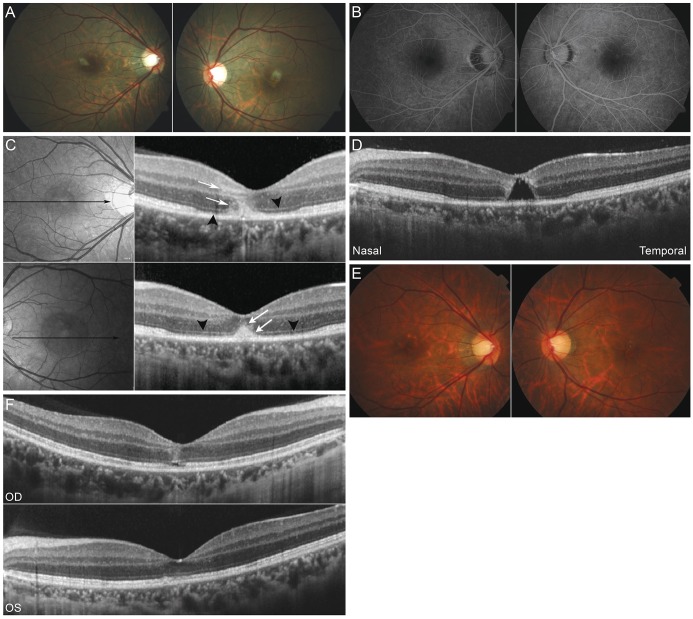
Fundus images showing the clinical course of the patient. (A) Small white infiltrations with hemorrhage were present in the juxtafovea of both eyes. (B) Fluorescein angiography showed no active leakage. (C) Spectral domain-optical coherence tomography showed disruption at the junction of the photoreceptor inner and outer segments and cone outer segment (black arrowheads). These changes were far more prominent and extensive in the left eye. Hyperreflective intraretinal deposits were present involving both the inner and outer retinal layers (white arrows). (D) Focal area of near total retinal tissue defect similar to an impending macular hole in the juxtafovea of the left eye. (E) Two weeks after intravenous antibiotic therapy, the intraretinal infiltrations were no longer visible. (F) Spectral domain-optical coherence tomography showed near full restoration of inner and outer segments junction and cone outer segment lines except for small focal defects at the fovea. Hyperreflective intraretinal infiltrations had decreased substantially. OD = right eye; OS = left eye.
On the second visit 2 weeks after appropriate intravenous antibiotic therapy, his BCVA had improved to 20 / 22 in right eye and 20 / 30 in left eye. Fundus examination showed complete resolution of the hyperreflective intraretinal deposits in both eyes (Fig. 1E). Spectral domain-optical coherence tomography showed near full restoration of the previously disrupted IS/OS junction and cone outer segment lines except for a small focal defect of the IS/OS junction in the left eye. The hyperreflective intraretinal deposits in both eyes were no longer present (Fig. 1F). Three months later, his BCVA were 20 / 20 in right eye and 20 / 40 in left eye; however, the focal defect of the IS/OS junction in the left eye was nearly unchanged, and the continuity of each retinal layer remained incomplete.
Although the incidence of macula-involving metastatic infection secondary to bacterial septic embolism is rare, careful observation is required when performing fundus examination for possible metastatic infection in bacteremia patients. Metastatic septic emboli may involve both the outer and inner retinal layers at the bilateral fovea and may cause a near total retinal tissue defect close to that of an impending macular hole. Our case showed that a macula-involving metastatic infection can involve reversible retinal structural change with no functional sequelae and improvement of visual acuity after suitable antibiotic therapy.
Notes
No potential conflict of interest relevant to this article was reported.