Changes in the Accommodation-convergence Relationship after the Artisan Phakic Intraocular Lens Implantation for Myopic Patients
Article information
Abstract
Purpose
To evaluate the change of accommodation-convergence parameters after implantation of Artisan phakic intraocular lens (PIOL).
Methods
Prospective study for the patients with the Artisan PIOL implantation was performed. A total of 37 patients (3 males and 34 females) enrolled the study. Preoperatively, convergence amplitude, the stimulus accommodative convergence per unit of accommodation (AC/A) ratio and the near point of convergence (NPC) were evaluated. After the Artisan PIOL implantation, the identical evaluations were repeated at 1 week, 1, 3, and 6 months after the surgery.
Results
Mean age was 24.3 ± 4.8 years old, and preoperative refractive error was -8.92 ± 4.13 diopters (D). After the implantation, mean refractive errors significantly decreased to within ±1.00 D, and noticeable complications were not found. The convergence amplitude and the stimulus AC/A ratio increased 1 month after the surgery, but progressively stabilized afterward to near preoperative values. NPC didn't show any significant change over follow-up period up to 6 months.
Conclusions
These results regarding implantation of the Artisan PIOL revealed the increase of accommodation-convergence relationship within first 1 month after the surgery, but progressive stabilization was noted during follow-up periods.
Various types of refractive surgery are becoming increasingly popular to those seeking an alternative to wearing glasses [1]. Besides excimer laser photorefractive keratectomy and laser in-situ keratomileusis (LASIK), implanting an intraocular lens in a phakic eye has become one of the most attractive surgical options for myopia correction [2]. For severe myopia patients, the excimer laser technology may be considered unsuitable because of anatomical structure incompatibility resulting in correction instability, haze, and corneal ectasia [2]. However, phakic intraocular lens (PIOL) implantation has opened an alternative way to correct the myopia without structural complications related to the excimer laser. The implantation of Artisan PIOL is considered a stable, safe method to correct moderate and severe myopia if strict inclusion criteria are applied [3].
The implantation of Artisan PIOL produced a state of near emmetropia in a patient with previous myopia, increasing the amount of accommodation required for near vision. In addition, in the absence of the prismatic effect of concave glasses, the convergence required for near fusion is also altered in myopia [4]. Due to these conditions, patients with the Artisan PIOL implantation might experience asthenopic symptoms such as double vision and blurring immediately after surgery. However, little has been described regarding the change in the accommodation-convergence relationship after Artisan PIOL implantation.
This study was designed to evaluate accommodation-convergence related parameters such as accommodative convergence per unit of accommodation (AC/A) ratio, convergence amplitude, and near point of convergence (NPC) change following the Artisan PIOL implantation.
Materials and Methods
Patients who visited the B & VIIT Eye Clinic, Seoul, Korea were recruited for this study. Thirty-seven patients who underwent implantation of an Artisan PIOL by the same surgeon (JKK) at B & VIIT Eye Clinic from December 2006 to June 2007 were enrolled. All procedures conformed to the tenets of the Declaration of Helsinki. During the study periods, there was no institutional review board in our hospital, so informed consent was obtained from the participants after explanation of the study. Exclusion criteria were those with manifest tropia, a history of strabismus surgery, absent binocular vision, and anterior segment pathologic condition.
Preoperative examination included uncorrected visual acuity (UCVA) and best-corrected visual acuity (BCVA) with Snellen chart, slit-lamp biomicroscopy, intraocular pressure, corneal keratometry, pupil diameter, iris configuration, and indirect ophthalmoscopic examination. Complementary evaluations included: corneal topography (Orbscan II; Bausch & Lomb, Rochester, NY, USA), axial length, anterior chamber depth with ultrasound, and central endothelial cell count (SP8000; Konan, Hyogo, Japan).
Stimulus AC/A ratio was assessed using the gradient method, previously described by von Noorden and Campos [5]. Through fully corrected glasses, the baseline angle of ocular alignment for the accommodative target at 6 m was measured with the alternate prism cover test. Afterward, upon placing a -3 diopters (D) lens before the eyes with full correction, the deviated angle was measured. The measurements were repeated three times, and the average of the measurements was considered to be the representative value. The convergence amplitude was measured using a handheld rotary prism. Placing it before the eye, a near (33 cm) target of Snellen E chart, size of 20 / 200, was fixed, and at a speed of 4 prism/sec, the prism was rotated. As the prism rotated, the moment of diplopia appearance was defined as a 'break point,' and the moment after the break point where the diplopia disappears was defined as a 'recovery point.' NPC was assessed as previously described by Maples and Hoenes [6]. A Bernell Accommodative Rule, which is commonly used in research, was utilized [7]. One end of the accommodative rule was placed just above the nose at the brow, between the two eyes. NPC measurements were repeated three times and the average of the measurements was considered to be the representative value.
Surgical procedure
The surgery was performed by the same surgeon (JKK), and the surgical protocol was identical in all cases. A week before the surgery, laser peripheral iridotomy was performed at the 12 o'clock direction on a candidate eye for preventing pupillary block glaucoma. Antibiotics and fluorometholone eye drops were administered four times a day until the day before the surgery.
All procedures were performed under local anesthesia with peribulbar injection. With a main scleral tunnel incision at 12 o'clock and two lateral paracentesis at 10 and 2 o'clock, the lens was introduced into the anterior chamber and enclavated to the iris at 3 and 9 o'clock meridians. Viscoelastics were used to maintain the depth of the anterior chamber and removed just before wound tightening. The incision was closed with 10-0 nylon interrupted suture and postoperative medications, including topical antibiotics and steroids, were maintained over four weeks after the surgery.
Postoperative examination
All patients were examined on the first postoperative day, and then one, two, and four weeks after surgery. The following examination schedule proceeded at the patient's convenience and condition. Visual acuity, tonometry, slit-lamp examination, endothelial specular microscopy, and indirect ophthalmoscopy were included in a routine examination upon follow-up. Residual refractive errors, UVCA, BCVA, and AC/A ratio were assessed at one week, then one, three, and six months after the surgery. Postoperative AC/A ratios were assessed without spectacle correction.
Data analysis
Statistical analysis was performed with the Wilcoxon's signed-ranks test. A p-value of less than 0.05 was considered significant. The IBM SPSS Statistics for Windows ver. 20.0 (IBM Corp., Armonk, NY, USA) was used for all statistical calculations.
Results
A total of 37 patients followed the study. The mean age of three men and 34 women was 24.3 ± 4.8 years old, ranging from 19 to 34 years. The preoperative refractive error (RE) ranged from -5.75 D to -11.25 D (mean, -8.92 ± 4.13 D) in spherical equivalent. Mean residual RE was -1.75 ± 1.47 in the right eye and -2.21 ± 2.57 in the left eye at postoperative one week, -0.75 ± 0.15 in the right eye and -0.64 ± 0.51 in the left eye at postoperative one month, and -0.50 ± 0.30 in the right eye and -0.52 ± 1.33 D in the left eye at postoperative three months. The mean residual RE was -0.54 ± 0.37 in the right eye and -0.57 ± 1.36 D in the left eye at six months after surgery. All values showed statistical significance compared to preoperative refractive error (p < 0.05).
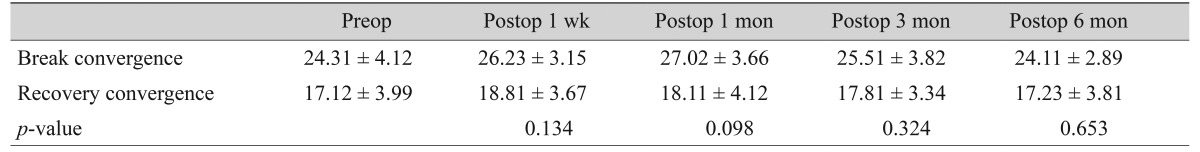
The convergence amplitude was measured as 24.31 ± 4.12/17.12 ± 3.99 (break/recovery) prism diopters (PD) before surgery. Upon six months of follow-up, the convergence amplitude showed only slight changes with statistical significance (Table 1).
The stimulus AC/A ratio showed changes after surgery. The preoperative stimulus AC/A ratio was 4.39 ± 0.79 PD/D. After one week and one month, the AC/A ratio (4.91 ± 1.22 PD/D at one week, 5.11 ± 0.71 PD/D at one month) increased with statistical significances (p < 0.05). However, afterward, the AC/A ratio seemed to stabilize, and was comparable at three or six months after surgery to the preoperative values (Fig. 1).
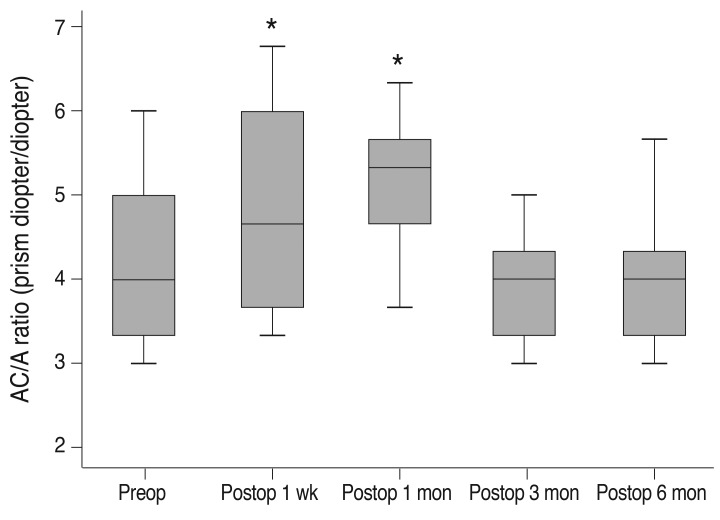
The stimulus accommodative convergence per unit of accommodation (AC/A) ratio before and after the implantation of Artisan phakic intraocular lens. Preop = preoperative; Postop = postoperative. *Statistically significant compared to preoperative value by Wilcoxon signed-rank test.
The preoperative NPC was 3.82 ± 1.37 cm. No significant differences in the NPC were observed at any of the follow-up visits, suggesting no effect of the Artisan PIOL implantation on the convergence power (Fig. 2).
Discussion
In this study, we evaluated the change in the accommodation-convergence parameters in myopic patients who had bilateral Artisan PIOL implantation. With their glasses removed, the patients may experience not only an improvement of visual acuity, but also a change in accommodation-convergence response required for daily activities.
There have been few reports describing alteration of the stimulus AC/A ratio after refractive surgery. After LASIK, no significant change of AC/A ratio between the group wearing glasses before surgery and naked after surgery have been reported [8]. Prakash et al. [4] reported a change in the stimulus AC/A ratio after bilateral LASIK following stabilization a few months after surgery. In the present study, we found an initial increase in the AC/A ratio early in the postoperative period. As previously reported, myopic individuals had a higher AC/A ratio than emmetropic individuals [9]. The residual RE after Artisan PIOL implantation might influence the AC/A ratio during the early postoperative period in this study. The residual RE one week postoperative was greater than the residual RE at postoperative one month, so it might be possible to underestimate the AC/A ratio at one week postoperative.
The stimulus AC/A ratio started to decrease at three months after the surgery, and progressively stabilized. This could be evidence of a stable accommodation-convergence relationship, which was altered after the Artisan PIOL implantation. We speculate the stabilization of the accommodation-convergence relationship would occur within the first three months after surgery.
The relation of AC/A ratio to refractive errors has been previously reported in numerous reports, revealing general increase in myopes. Rosenfield and Gilmartin [10] reported greater accommodative convergence and stimulus AC/A ratios in myopes than in emmetropes. In the younger population, myopic children had been found to have a reduced accommodation, whether measured in the laboratory [11,12] or clinic [13,14], which resulted in a greater AC/A ratio. Without emmetropic control group, these findings were impossible to reveal in this study. The AC/A ratio was increased for the first month, subsequently the AC/A ratio was decreased to the near the preoperative value. These findings might be due to unstable myopic residual refractive error during the initial postoperative period.
There might be possible explanations as to why the AC/A ratio was increased during early postoperative periods. Accommodation and vergence demands vary for ametropes depending on whether their refractive error is corrected with single vision contact lens or spectacle lens [15]. Increased accommodation and greater convergence effort are required when wearing contact lenses in myopic patients [16]. Thus, the AC/A ratio might be increased during the early postoperative period, because myopic patients remove their glasses after Artisan PIOL implantation.
In conclusion, this prospective study revealed a stabilization of the accommodation-convergence relationship after the Artisan PIOL implantation within three months postoperatively. Being newly adapted to emmetropic status, the patient seemed to accommodate more, thus increasing the convergence amplitude and stimulus AC/A ratio until one month postoperatively. However, the AC/A ratio gradually returned to near the preoperative value within six months. Larger studies are recommended to evaluate the difference of the AC/A ratio developed by different surgical techniques to correct myopia. Furthermore, the effect of residual refractive error change on the AC/A ratio would be worthwhile to evaluate.
Notes
This study was originally presented as a poster at the Association for Research in Vision and Ophthalmology meeting which was held in Fort Lauderdale, Florida, USA on May, 2007.
No potential conflict of interest relevant to this article was reported.