 |
 |
| Korean J Ophthalmol > Volume 27(2); 2013 > Article |
Abstract
Purpose
To determine the correlation between renal dysfunction and the morphologic changes of macular edema in diabetes.
Methods
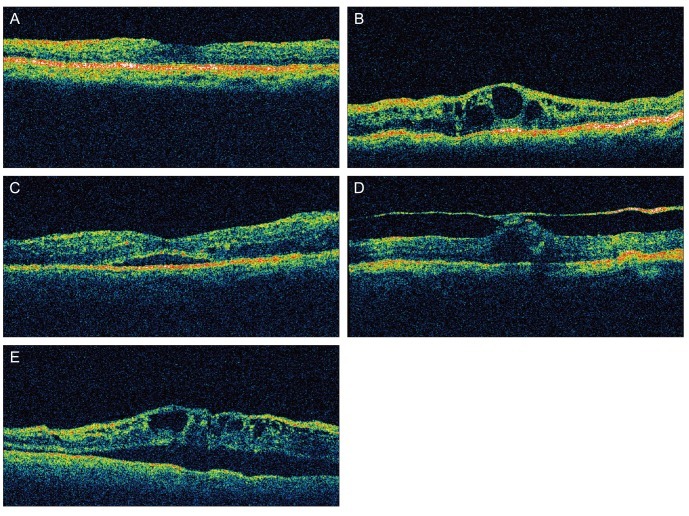
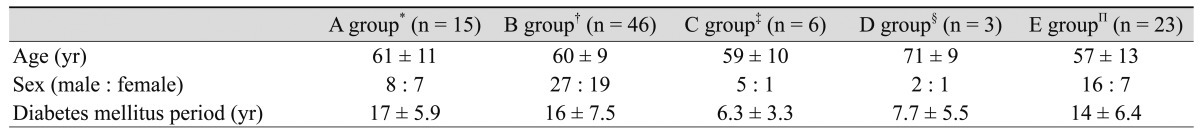
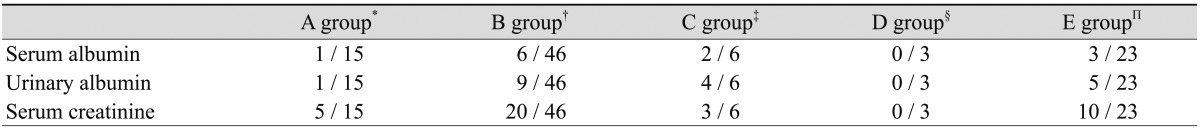
The current study included 93 patients with diabetic macular edema based on optical coherence tomography (OCT) who completed systemic condition testing one month before or after the OCT. Based on the OCT findings, patients were divided into the following five groups: group A (diffuse), group B (cystoid), group C (serous), group D (vitreomacular tractional), and group E (a mixed presence of cystoid and serous types). In each group, we performed a retrospective analysis of serum albumin, urine albumin, and serum creatinine. We also analyzed the patients in whom serum albumin was <3.0 mg/dL and serum creatinine was >1.6 mg/dL. Urine albumin was measured in all five groups. In each group, a comparative analysis was performed using Fisher's exact test.
Results
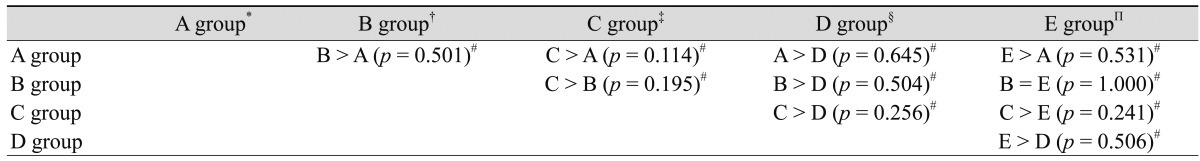
The number of patients who were assigned to groups A to E was 15, 46, 6, 3, and 23, respectively. According to a comparison of the patients in whom the serum albumin and serum creatinine were abnormal, there was no significant difference among the five groups. The proportion of patients in whom the urine albumin was abnormal was significantly greater in group C (67%) than in groups A (7%), B (20%), or E (22%).
In patients with diabetes mellitus, diabetic macular edema is one of the major causes of loss of visual acuity. Macular edema occurs as result of increased permeability of retinal capillary vessels due to disruption of the blood-retinal barrier. With the common use of optical coherence tomography (OCT), the morphology of diabetic macular edema has been classified into various types [1,2]. Otani et al. [2] reported that macular edema can be classified into diffuse, cystoid, serous, and mixed types. Serous-type macular edema occurs in 15% to 30% of diabetic macular edema cases [3]. To date, however, a limited number of studies have been conducted to determine the basis for the differences in morphologic type of diabetic macular edema. In particular, the relationship between diabetic macular edema type and non-ocular factors has not been studied. Thus, we studied the relationship between renal dysfunction and the morphologic changes in macular edema in patients with diabetes mellitus.
Of the diabetes mellitus patients who attended our out-patient clinic in the Department of Ophthalmology from January 2003 to June 2010, 93 were enrolled in the current study. The inclusion criteria were as follows: the presence of diabetic macular edema on OCT (Stratus OCT; Carl Zeiss Meditec, Dublin, CA, USA), and systemic condition test performed one month before or after the OCT. Based on the OCT findings, the patients were divided into the following five groups: group A (diffuse), group B (cystoid), group C (serous), group D (vitreomacular tractional), and group E (mixed presence of cystoid and serous types) (Fig. 1). In each group, we performed a retrospective analysis of serum albumin, urine albumin, and serum creatinine levels. In addition, we also analyzed the patients in whom serum albumin was <3.0 mg/dL, serum creatinine was >1.6 mg/dL and who had albuminuria. In each group, a comparative analysis was performed using Fisher's exact test. The exclusion criteria were type 1 diabetes mellitus, uncontrolled hypertension with medication, laser photo-coagulation history and proliferative diabetic retinopathy. The patients with different types of macular edema in both eyes and confusing cases due to bad image quality on OCT were also excluded.
Groups A to E contained 15, 46, 6, 3, and 23 patients, respectively. The respective mean ages of the patients in each group were 61, 60, 59, 77, and 57 years. All patients had non-insulin-dependent diabetes mellitus. The gender distribution was as follows: group A, 8 men and 7 women; group B, 27 men and 19 women; group C, 5 men and 1 woman; group D, 2 men and 1 woman; and group E, 16 men and 7 women. The mean duration of diabetes was 17, 16, 6.3, 7.7, and 14 years in groups A to E, respectively (Table 1). The mean serum albumin level was 3.94, 3.83, 3.31, 4.13, and 3.63 mg/dL in groups A to E, respectively. The mean serum creatinine level was 2.90, 2.53, 3.41, 1.03, and 2.64 mg/dL in groups A to E, respectively (Table 2). The number of patients in whom the serum albumin level was abnormal was 1, 6, 2, 0, and 3 in groups A to E, respectively. The number of patients in whom the urine albumin was abnormal was 1, 9, 4, 0, and 5 in groups A to E, respectively. Furthermore, the number of patients in whom the serum creatinine was abnormal was 5, 20, 3, 0, and 10 in groups A to E, respectively (Table 3).
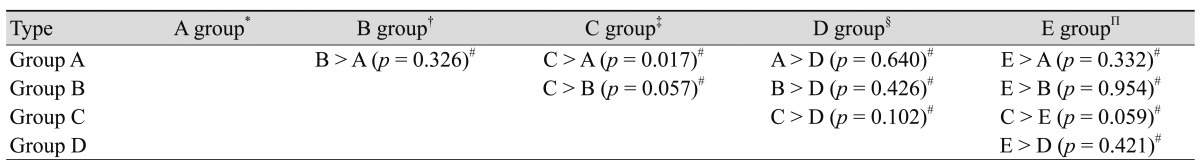
A comparison of the patients in each group in whom the serum albumin level was lower than the normal value showed that the highest serum albumin value was in group C; however, this difference did not reach statistical significance (Table 4). In addition, a comparison of the patients who had albuminuria showed the highest proportion in group C. Between groups C and A, there was a significant difference in the urine albumin level (p = 0.017) (Table 5).
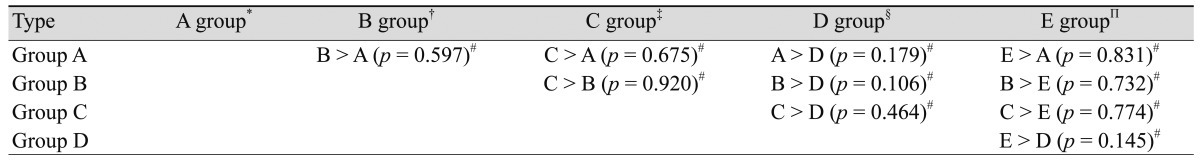
A comparison of the patients in whom serum creatinine was higher than the normal value showed that the highest mean serum creatinine level was in the group C; however, the difference was not statistically significant (Table 6).
Since the development of OCT, a diagnosis of diabetic macular edema can be made easily even though diabetic macular edema cannot be detected on examination of the fundus. The treatment effects can also be easily evaluated. Based on OCT findings, the morphologies of macular edema can be subdivided and objectively classified. There is variability of treatment effects of intravitreal injection depending on the morphology of macular edema. It has also been reported that the prognosis of visual acuity varies depending on the morphology of macular edema [1].
In the current study, attempts were made to identify the relationship between the morphology of macular edema and systemic conditions using three different tests. In group D (vitreomacular tractional type), there were no patients in whom the three clinical parameters were abnormal. These results indicate that types of diabetic macular edema other than vitreomacular tractional types are to some extent associated with systemic conditions. The proportion of patients in group C (serous type) in whom albuminuria was detected was significantly higher than that in group A (diffuse type). Despite a lack of statistical significance, albuminuria in patients with serous-type diabetic macular edema, as compared with group B (cystoid type) or E (a mixed presence of the serous and cystoid types), might be associated with renal function as a non-ocular factor. This finding may be due to the decreased intravascular osmotic pressure because of the excretion of urinary albumin.
Several hypotheses have been proposed to explain the pathophysiology of serous-type macular edema. According to Kang et al. [1], in patients with serous-type diabetic macular edema, albumin and other body fluids leak into the subretinal space through an external limiting membrane because of destruction of the inner blood retinal barrier. Kang et al. [1] also noted that macular edema occurs when these substances cannot be effectively cleared. In addition, Gaucher et al. [4] maintained that serous-type retinal edema can occur in the early stage of pathogenesis of diabetic macular edema, and this can be seen prior to the accumulation of a massive amount of fluid in the macular region. However, serous-type macular edema in patients with diabetic retinopathy was not associated with a greater severity of diabetic macular edema.
Our results show a significantly higher frequency of serous-type macular edema in patients with albuminuria. Despite a lack of statistical significance, serous-type macular edema usually occurred in patients with a lower level of serum albumin. These results indicate that serous-type macular edema might have a relationship with the excretion of albumin into the urine due to decreased renal function. It is also presumed that the excretion of albumin and the decreased concentration of serum albumin cause an overload of body fluids and decreased intravascular osmotic pressure, which leads to the occurrence of serous-type macular edema.
Romero et al. [5] reported a correlation between macular edema and microangiopathy of the kidney in patients with type I diabetes mellitus. Romero et al. [5] reported that various factors are associated with the occurrence of diabetic macular edema, and compulsive management of clinical parameters, such as blood glucose, low density lipoprotein (LDL)-cholesterol, and blood pressure, can reduce the occurrence of macular edema. Romero et al. [5] also noted that there was no significant correlation between microangiopathy of the kidney and macular edema. While the correlation between microproteinuria and macular edema was not significant in normal diabetes patients, it was significant in patients with severe renal dysfunction. Thus, a greater severity of renal dysfunction is correlated with the occurrence of macular edema. The reports are based on a 15-year, follow-up study conducted with patients who did not have diabetic retinopathy or nephropathy. In our study, however, the clinical examination confirmed the correlation between renal function and the morphology of diabetic macular edema. The correlation between renal function and serous-type macular edema could be confirmed by considering other systemic factors that might affect diabetic macular edema, including blood pressure, LDL-cholesterol, or HbA1C. Further studies are warranted to determine whether or not the morphology of macular edema varies depending on the level of systemic parameters not directly associated with systemic edema, such as blood pressure, LDL-cholesterol, or HbA1C.
As the current results showed, there is the possibility that serous-type macular edema might have a relationship with the excretion of albumin in the urine. In association with this, retinopathy accompanied by nephropathy would be a serous type. However, this occurrence might not be edema caused by increased permeability due to diabetic retinopathy but secondary retinal edema due to systemic edema. In this paper, systemic edema is referred to as a condition in which there is an overload of body fluids compared to the normal level. Thus, an overload of body fluids compared to the normal level is common in patients with diabetic nephropathy serous-type retinal edema would occur in the macular region. Group D represents an edema that mainly occurs as a result of physical traction and is not directly associated with vascular leakage in the retina; the edema is therefore not associated with renal dysfunction. In groups A and B, if there is diabetic retinopathy, the corresponding diabetic nephropathy would concurrently occur and result in an abnormal blood test. In group C, systemic edema due to diabetic nephropathy, as well as diabetic retinopathy, contributed to the occurrence of macular edema.
Ciardella [6] reported mixed-type serous and cystoid macular edema in patients who excrete urine albumin. Ciardella [6] speculated that the excretion of albumin in the urine appeared due to an overload of body fluids in the macular region. He also noted that the macular edema was treated with the systemic administration of diuretics for correction of the overload. This suggests that an overload of body fluids accompanied by renal dysfunction appears as serous or mixed type macular edema that can be treated by correcting the overload of body fluids.
In addition, if the morphology of diabetic retinal edema was due to systemic differences, the treatment of systemic edema, such as diuretics, would be one of the treatment modalities for diabetic macular edema.
The limitations of the current study are as follows. First, the study was conducted retrospectively. Second, the number of patients assigned to each group varied. Third, although there was statistical significance with regard to urinary albumin excretion, there was a higher prevalence of abnormalities in cases of serous macular edema compared with the other groups. Other clinical parameters that might indicate systemic vascular events deserve further study in a larger population of patients.
REFERENCES
1. Kang SW, Park CY, Ham DI. The correlation between fluorescein angiographic and optical coherence tomographic features in clinically significant diabetic macular edema. Am J Ophthalmol 2004;137:313-322.


2. Otani T, Kishi S, Maruyama Y. Patterns of diabetic macular edema with optical coherence tomography. Am J Ophthalmol 1999;127:688-693.


3. Ozdemir H, Karacorlu M, Karacorlu S. Serous macular detachment in diabetic cystoid macular oedema. Acta Ophthalmol Scand 2005;83:63-66.


4. Gaucher D, Sebah C, Erginay A, et al. Optical coherence tomography features during the evolution of serous retinal detachment in patients with diabetic macular edema. Am J Ophthalmol 2008;145:289-296.


Fig. 1
Five different patterns of diabetic macular edema on optical coherence tomography. (A) Diffuse type of macular edema, (B) cystoid type of macular edema, (C) serous type of macular edema, (D) vitreomacular tractional type of macular edema, and (E) mixed type of macular edema.




 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




