 |
 |
| Korean J Ophthalmol > Volume 27(1); 2013 > Article |
Abstract
Purpose
To evaluate changes over time of the anterior capsule opening size after phacoemulsification, based on haptic number and composition of three acrylic intraocular lenses (IOLs).
Methods
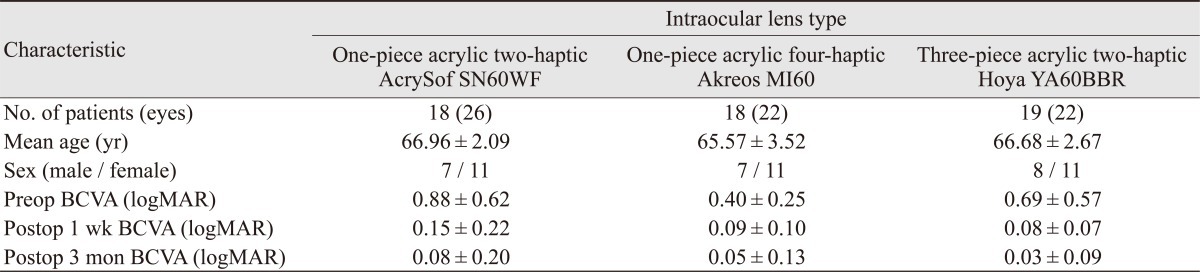
Fifty-five patients (70 eyes) were included. All underwent phacoemulsification followed by implantation of either an acrylic IOL with two-haptic (one-piece, 26 eyes; three-piece, 22 eyes), or four-haptic (one-piece, 22 eyes). The area of the anterior capsule opening size was measured one week postoperatively (baseline) and at three months.
Recent advances in cataract surgery and the development of various intraocular lenses (IOLs) have improved patient satisfaction. However, anterior capsule contraction is still an unavoidable post-operative complication, reducing visual acuity and resulting in refractive changes. Anterior capsule contraction begins when the capsulorhexis leaf settles on the optic surface after continuous curvilinear capsulorhexis (CCC) [1,2]. The anterior lens epithelial cells (LECs) remaining on the anterior capsule leaf are known to proliferate on the IOL surface after CCC and also undergo myofibroblastic transdifferentiation. The precise mechanism has not been established yet. It is believed that the degree of anterior capsule contraction is related to many factors, including the lens capsular or zonular state of the patient, concurrent ocular pathology such as retinitis pigmentosa, pseudoexfoliation, diabetic retinopathy, high myopia, uveitis, pars planitis, myotonic dystrophy, surgical complications and advanced age. It has also been associated with conditions such as cataract surgery combined with trabeculectomy, diseases of intraocular inflammation, blood-aqueous barrier compromise, and IOL material and morphology [3-7].
Reduction of the equatorial capsular bag diameter, malposition of the anterior capsule opening, anterior subcapsule opacification, hyperopic shift, PC IOL displacement or encapsulation, zonular traction, ciliary body detachment with resultant hypotony, and retinal detachment are included in the secondary complications of capsular contraction syndrome (CCS) [8]. Although it does not appear to affect pathologic conditions, portions of the entering light are intercepted by the constricted anterior capsule rim, which may decrease contrast sensitivity [9]. Even if the contraction of the anterior capsule opening may not markedly impair visual function, it frequently disturbs visualization and photocoagulation of the peripheral retina.
Composition of the implanted IOL is also thought to influence the degree of anterior capsule contraction. Several previous studies reported that anterior capsule contraction after implantation of a silicone optic IOL was more extensive than that after implantation of either polymethyl methacrylate (PMMA) or acrylic optic IOLs [8,10,11]. Kim et al. [12] reported that because of the stability of IOLs of the four-haptic design, four-haptic IOL implantation showed significantly less elevation of early postoperative IOP and higher accuracy of IOL power than those of two-haptic IOL implantation in combined surgery (phacoemulsification, intraocular lens insertion, and vitrectomy). Therefore, we suggested that a larger interfacial plane of a four-haptic lens might reduce epithelial cell growth on the anterior capsule, possibly by leading to constant tension on the zonular fiber. This may also enhance the overall stability of the IOL within the eye. Research has been conducted on new IOL to reduce such complications, yet no study has been done on whether four-haptic IOL versus two-haptic IOL reduces anterior capsule contraction by promoting capsule stability. There have been few previous studies to assess influence of the haptic materials on anterior capsule contraction. In this study, we compared the changes in the area of the anterior capsule opening with three types of IOLs with different haptic factors.
Fifty-five patients (70 eyes) who underwent cataract surgery from September 2009 to May 2010 at Uijeongbu St. Mary's Hospital, The Catholic University of Korea, were included in this study. The study protocol was reviewed and approved by the institutional review board. All were of Korean race. Patient characteristics are shown in Table 1. Exclusion criteria were previously recognized risk factors for anterior capsule shrinkage such as ocular pathology including retinitis pigmentosa, pseudoexfoliation syndrome, history of intraocular surgery or inflammation, diabetes mellitus requiring medical control, glaucoma, high myopia and pupillary diameter of <6.0 mm after mydriasis.
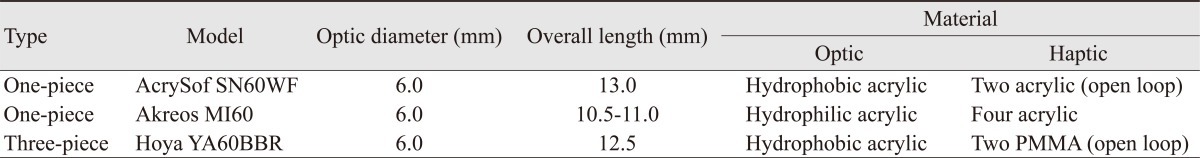
Study participants were divided into three groups, with all patients receiving an acrylic IOL. Three types of acrylic IOL were inserted. One-piece two-haptic IOL (Acrysof IQ SN60WF; Alcon, Fort Worth, TX, USA) were classified as group I, one-piece four-haptic IOL (Akreos AO MI60; Bausch & Lomb, Rochester, NY, USA) as group II, and three-PMMA piece two-haptic IOL (Hoya YA60BBR; Hoya, Tokyo, Japan) as group III, based on type of IOL inserted (Tables 1 and 2).
Each cataract surgery was performed by the same surgeon (SYK) in a standardized fashion. The anterior chamber was filled with a viscoelastic substance and a well-centered round continuous curvilinear capsulorrhexis measuring approximately 5.0 mm in diameter was accomplished. Continuous curvilinear capsulorhexis slightly smaller than the IOL optic diameter was created to overlie the IOL optic circumferentially.
Anterior segment image was taken after displaying the anterior capsule by retroillumination after mydriasis at one week and three months after cataract surgery. The area of the anterior capsule opening was calculated by the image analysis program. The percent reduction of the area at three months after surgery was calculated based upon the area measured at one week after surgery (percentage contraction at three months = [anterior capsule opening area at one week - anterior capsule opening area at 3 months] / anterior capsule opening area at one week ├Ś 100). The data were analyzed by multiple comparisons using the t-test and ANOVA (SPSS ver. 12.0.1; SPSS Inc., Chicago, IL, USA). A p-value <0.05 was considered statistically significant.
Average patient age was 62 years. There were 22 men and 33 women. Table 3 and Fig. 1 show the rate of reduction in the area of the anterior capsule opening. The initial area of the anterior capsule opening one week after surgery was not significantly different among the groups (p = 0.88). There was a significant reduction at three months compared to one week in all three groups (p < 0.001). Differences among one-piece acrylic two-haptics, one-piece acrylic four-haptics and three-piece PMMA two-haptic acrylic IOLs were compared by calculating the rate of area reduction at three months versus one week postoperatively. However, there was no significant difference in shrinkage of the anterior capsule among the three groups (p = 0.36).
CCC possesses many advantages such as reducing the posterior capsule opacity and strengthening the stability of IOL in lens capsule. On the other hand, it can cause complications such as capsular bag distention, anterior capsule contraction, opacity, and IOL drop in vitreous after neodymium-YAG laser capsulotomy [1,2,13]. Nishi and Nishi [14] reported that fibrous metaplasia on IOL formed only in portions contacting the anterior surface of PCL. Anterior capsule contraction is said to occur when LEC remaining on the IOL surface proliferate and undergo fibrous metaplasia in contacting the IOL. In other words, postoperatively, residual LECs are stimulated to produce cytokines that may affect the epithelial cells, inducing collagen production and fibrous proliferation. If an exaggerated response occurs, it can lead to capsule contracture syndrome.
Immunohistochemistry shows that fibroblast-type LECs proliferate and form extracellular matrix containing various collagen types, fibronectin, and osteopontin by receiving inflammatory cytokine signals secreted due to trauma from CCC or stimulus from contact with IOL [5,15-17]. Contraction of the anterior capsulorhexis supposedly occurs when centripetal forces exceed centrifugal forces, which act on both zonules and the capsulorhexis edge. When visual function of the patient is disturbed substantially because of this constriction, a neodymium: yttrium-aluminum-garnet laser anterior capsulotomy becomes necessary. However this procedure may increase the risk of cystoids macular edema, retinal detachment, damage to the IOL, and corneal endothelial cell damage. Even after YAG laser anterior capsulotomy, it is still difficult to observe peripheral retina during fundic examination or vitrectomy [18-21].
The area of the anterior capsule opening shrinks rapidly during the first month and more slowly thereafter. The reduction in the area of the anterior capsule opening did not progress after three months in any IOL group [22]. In one study, LECs proliferated actively until three months postoperatively, supporting the hypothesis that anterior capsule contraction is a result of LEC proliferation [22]. Also in this study, statistically significant anterior capsule contraction occurred during three months in all three groups. There have been many studies about the relationship between IOL and anterior capsule contraction. One of these studies reported that anterior capsule contraction in the eyes with a silicone or hydrogel optic IOL was more extensive than that in the eyes with a PMMA or acrylic optic IOL [8,10,11]. The association of silicone and hydrogel optics with greater anterior capsule contraction can be explained by lesser adhesion of the optic materials to the lens capsule. Weak adhesion of these optic materials to the capsule would allow space for active proliferation of LECs and for synthesis of extracellular matrix [23]. In contrast, because the acrylic optics adhere firmly to the capsule, and remnant LECs are minimally exposed to various cytokines in aqueous humor, fibrosis and contraction of the anterior capsule would not be as extensive [24,25]. The morphology of IOL also has an influence. Anterior capsule contraction is more likely to occur with plate haptic IOLs or IOLs with a thin optic that cause less capsule dilation of the centrifugal haptics [7,26]. Meanwhile, Miyake et al. [27] found that hydrophobic lenses induce greater postoperative inflammation and more anterior capsule opacification than hydrophilic IOLs. Tsinopoulos et al. [28] reported that incidence of anterior capsule contraction syndrome was significantly greater after hydrophilic IOL implantation compared with hydrophobic lenses. Gallagher and Pavilack [29] reported that polypropylene haptics IOL and the PMMA haptics IOL did not differ significantly in their ability to prevent CCS. According to Hayashi and Hayashi [30], no significant difference was observed in percent reduction between round-edge and sharp-edge optic acrylic IOLs. In our study, the reduction at three months in the area of the anterior capsule opening was not different between one-piece acrylic lens and three-piece acrylic lens or between four-haptic lens and two-haptic one-piece acrylic lens. This finding agrees with that of Park et al. [31], who reported no significant difference between one-piece and three-piece acrylic lenses.
Recent studies suggest the four-haptic design shows slightly better intraoperative and postoperative centration than two-haptic IOL, although the differences did not reach the level of statistical significance in combined phacoemulsification and pars plana vitrectomy. The four-haptic IOLs may provide a large IOL surface in contact with posterior capsule and a more accurate IOL fixation in the capsular bag, leading to a constant tension on the zonular fibers and less myopic shift [12,32]. This led to the assumption of this study that the stability of four-haptic IOL lessens anterior capsule contraction, but the haptic number and design were not strongly related to anterior capsule contraction.
The mean difference in the percentage of area reduction between the IOLs with silicone and acrylic optics was approximately 5% [30]. However, the difference between the percentage in healthy eyes and those with other conditions was approximately 40% in eyes with retinitis pigmentosa, 15% in eyes with pseudoexfoliation syndrome, and 14% in eyes with diabetic retinopathy [4,5]. We should consider appropriate IOL selection and techniques such as intraoperative removal of LECs in reducing anterior capsule opening contraction, especially in patients at high risk for contraction.
In conclusion, there was no significant difference of reduction in the anterior capsule opening between one-piece two-haptics, one-piece four-haptics and three-piece PMMA two-haptics acrylic IOLs. The material and number of haptics of the three IOLs did not influence the degree of anterior capsule opening shrinkage. Further studies are necessary to investigate which IOL reduces anterior capsule contraction in a larger patient group.
REFERENCES
1. Hansen SO, Crandall AS, Olson RJ. Progressive constriction of the anterior capsular opening following intact capsulorhexis. J Cataract Refract Surg 1993;19:77-82.


3. Hayashi K, Hayashi H, Matsuo K, et al. Anterior capsule contraction and intraocular lens dislocation after implant surgery in eyes with retinitis pigmentosa. Ophthalmology 1998;105:1239-1243.


4. Hayashi H, Hayashi K, Nakao F, Hayashi F. Anterior capsule contraction and intraocular lens dislocation in eyes with pseudoexfoliation syndrome. Br J Ophthalmol 1998;82:1429-1432.



5. Hayashi H, Hayashi K, Nakao F, Hayashi F. Area reduction in the anterior capsule opening in eyes of diabetes mellitus patients. J Cataract Refract Surg 1998;24:1105-1110.


6. Ursell PG, Spalton DJ, Pande MV. Anterior capsule stability in eyes with intraocular lenses made of poly(methyl methacrylate), silicone, and AcrySof. J Cataract Refract Surg 1997;23:1532-1538.


7. Gonvers M, Sickenberg M, van Melle G. Change in capsulorhexis size after implantation of three types of intraocular lenses. J Cataract Refract Surg 1997;23:231-238.


8. Hayashi K, Hayashi H, Nakao F, Hayashi F. Anterior capsule contraction and intraocular lens decentration and tilt after hydrogel lens implantation. Br J Ophthalmol 2001;85:1294-1297.



9. Hayashi K, Hayashi H. Effect of anterior capsule contraction on visual function after cataract surgery. J Cataract Refract Surg 2007;33:1936-1940.


10. Cochener B, Jacq PL, Colin J. Capsule contraction after continuous curvilinear capsulorhexis: poly(methyl methacrylate) versus silicone intraocular lenses. J Cataract Refract Surg 1999;25:1362-1369.


11. Dahlhauser KF, Wroblewski KJ, Mader TH. Anterior capsule contraction with foldable silicone intraocular lenses. J Cataract Refract Surg 1998;24:1216-1219.


12. Kim JW, Yang JW, Jee DH. Stability of four-haptic intraocular lens in combined phacoemulsification and vitrectomy. J Korean Ophthalmol Soc 2010;51:829-834.

13. Davison JA. Capsular bag distension after endophacoemulsification and posterior chamber intraocular lens implantation. J Cataract Refract Surg 1990;16:99-108.


14. Nishi O, Nishi K. Intraocular lens encapsulation by shrinkage of the capsulorhexis opening. J Cataract Refract Surg 1993;19:544-545.


15. Meacock WR, Spalton DJ, Stanford MR. Role of cytokines in the pathogenesis of posterior capsule opacification. Br J Ophthalmol 2000;84:332-336.



16. Wormstone IM. Posterior capsule opacification: a cell biological perspective. Exp Eye Res 2002;74:337-347.


17. Kato S, Oshika T, Numaga J, et al. Anterior capsular contraction after cataract surgery in eyes of diabetic patients. Br J Ophthalmol 2001;85:21-23.



18. Spalton DJ. Posterior capsular opacification after cataract surgery. Eye (Lond) 1999;13(Pt 3b):489-492.


19. Weiblinger RP. Review of the clinical literature on the use of the Nd:YAG laser for posterior capsulotomy. J Cataract Refract Surg 1986;12:162-170.


20. Akerele T, Minasian M, Little B, Jagger J. Posterior dislocation of Staar plate haptic silicone lenses following Nd:YAG capsulotomy. Eye (Lond) 1999;13(Pt 5):700-702.


21. Michaeli-Cohen A, Belkin M, Goldring A, et al. Prevention of posterior capsule opacification with the CO2 laser. Ophthalmic Surg Lasers 1998;29:985-990.


22. Hayashi K, Hayashi H, Nakao F, Hayashi F. Reduction in the area of the anterior capsule opening after polymethylmethacrylate, silicone, and soft acrylic intraocular lens implantation. Am J Ophthalmol 1997;123:441-447.


23. Hayashi K, Hayashi H. Intraocular lens factors that may affect anterior capsule contraction. Ophthalmology 2005;112:286-292.


24. Oshika T, Nagata T, Ishii Y. Adhesion of lens capsule to intraocular lenses of polymethylmethacrylate, silicone, and acrylic foldable materials: an experimental study. Br J Ophthalmol 1998;82:549-553.



25. Nagata T, Minakata A, Watanabe I. Adhesiveness of AcrySof to a collagen film. J Cataract Refract Surg 1998;24:367-370.


26. Sickenberg M, Gonvers M, van Melle G. Change in capsulorhexis size with four foldable loop-haptic lenses over 6 months. J Cataract Refract Surg 1998;24:925-930.


27. Miyake K, Ota I, Miyake S, Maekubo K. Correlation between intraocular lens hydrophilicity and anterior capsule opacification and aqueous flare. J Cataract Refract Surg 1996;22(Suppl 1):764-769.


28. Tsinopoulos IT, Tsaousis KT, Kymionis GD, et al. Comparison of anterior capsule contraction between hydrophobic and hydrophilic intraocular lens models. Graefes Arch Clin Exp Ophthalmol 2010;248:1155-1158.


29. Gallagher SP, Pavilack MA. Risk factors for anterior capsule contraction syndrome with polypropylene or poly(methyl methacrylate) haptics. J Cataract Refract Surg 1999;25:1356-1361.


30. Hayashi K, Hayashi H. Comparison of the stability of 1-piece and 3-piece acrylic intraocular lenses in the lens capsule. J Cataract Refract Surg 2005;31:337-342.


Fig.┬Ā1
This graph shows postoperative changes in the area of the anterior capsule opening (ACO). The initial area of the ACO one week after surgery was not significantly different among the groups (p = 0.88). There was a significant reduction at three months compared to one week in all three groups (p < 0.001). However, there was no significant difference in ACO three months postoperatively among the three groups (p = 0.65). *Statistically significant (p < 0.05).





 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




