Bilateral Nongranulomatous Uveitis with Infective Endocarditis
Article information
Abstract
A 32-year-old male who had infective endocarditis complained of photophobia and blurred vision in both eyes. Biomicroscopic examination and fundus examination revealed anterior chamber reaction, vitritis, optic disc swelling, and Roth spots. He was diagnosed with bilateral nongranulomatous uveitis and treated with topical steroid eye drops and posterior sub-Tenon injection of triamcinolone. His visual symptoms were resolved within 1 week, and inflammation resolved within 4 weeks after treatment.
Infective endocarditis (IE) is a microbial infection of the endothelial surface of the heart. The authors report bilateral nongranulomatous uveitis with optic disc swelling in a patient with IE.
Case Report
A 32-year-old male presented tender papulopustules (Osler's node) on the pulp of right 2nd and left 3rd fingers for 14 days since June 2010. The patient had intermittent fever without any underlying systemic diseases. In July 2010, the patient was admitted to our institution, and physical examination revealed a grade III/IV pansystolic murmur over the apex. Transthoracic and transesophageal echocardiography showed vegetation in the anterior leaflet of the mitral valve and severe mitral regurgitation. Blood sample testing showed elevated erythrocyte sedimentation rate (91 mm/hr) with normal range anti-streptolysin O (ASO), and blood cultures were positive for Streptococcus parasanguinis (α-hemolytic streptococcus). With the diagnosis of IE, intravenous vancomycin 1 gm was injected every 12 hours for 4 weeks during hospitalization.
The patient complained of photophobia and blurred vision in both eyes 2 days after admission. Best-corrected visual acuity (BCVA) was 20 / 32 in both eyes. The biomicroscopic examination showed 2+ cells in the anterior chamber without keratic precipitates and vitritis in both eyes. Fundus examination showed optic disc swelling with multiple retinal hemorrhages with pale centers (Roth spots) (Fig. 1A). Fluorescein angiography showed hyperfluorescence in the optic disc and hypofluorescence in the Roth spots in both eyes (Fig. 1B). Goldmann visual field test showed Seidel scotoma in the right eye and paracentral scotoma in the left eye.
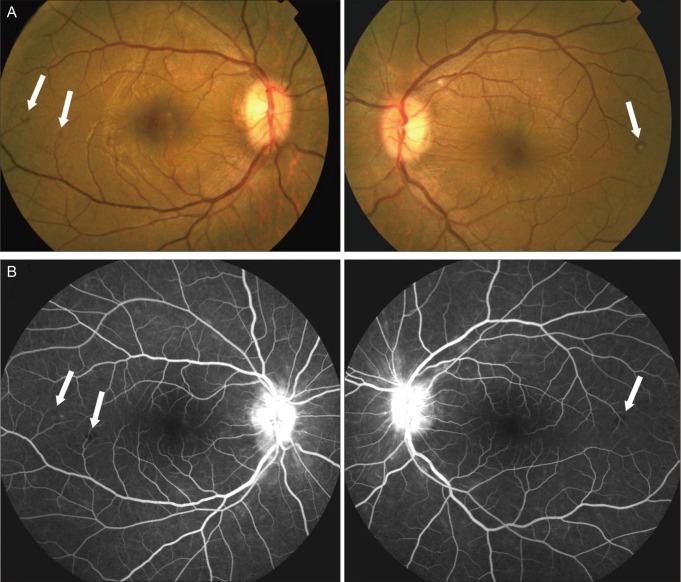
(A) At baseline, fundus photograph of both eyes showed optic disc swelling and retinal hemorrhages with pale centers (Roth spots) in the temporal retina (arrows). Best-corrected visual acuity was 20 / 32 in both eyes. (B) Fluorescein angiography showed hyperfluorescence in the optic disc and hypofluorescence in the Roth spots (arrows) in both eyes.
Serologic test for uveitis were negative including HLA B-27, antinuclear antibody, antinuclear cytoplasmic antibody, angiotensin converting enzyme, rheumatoid factor, and Venereal Disease Research Laboratory test. Pathergy test for Behcet's disease was also negative. With the diagnosis of bilateral nongranulomatous uveitis with optic disc swelling in IE, the patient was given topical 1% prednisolone acetate every 4 hours and cylcoplegics. In addition, the patient received a 40 mg (1 mL) posterior sub-Tenon injection of triamcinolone (Triam; Dongkwang Pharmacy, Seoul, Korea).
At 1 week after triamcinolone injection, BCVA increased to 20 / 20 in both eyes. Cells in the anterior chamber and vitritis resolved within 4 weeks after the injection. The fundus showed complete resolution of disc swelling with decreased retinal hemorrhages in both eyes.
Discussion
Ophthalmologic problems associated with IE are rare, although several cases of endophthalmitis have been reported [1,2]. The patients with endophthalmitis underwent valve replacement surgery, and their eyes showed hypopyon with visual acuity of light perception. Only one study reported uveitis in a patient with diabetes and IE, and the uveitis persisted for more than 3 months [3]. In all of the above studies, the causative organism was β-hemolytic group B streptococcus.
However, in the present case, the patient was a healthy male without underlying systemic diseases, and blood culture showed the previously unreported Streptococcus parasanguinis. In addition, uveitis with optic disc swelling resolved within 1 month after posterior sub-Tenon injection of triamcinolone.
Many studies reported uveitis with poststreptococcal syndrome, an autoimmune disorder precipitated by infection with group A streptococci [4,5]. However, in the present study, the patient showed no manifestations including acute rheumatic fever, reactive arthritis, or acute glomerulonephritis. In addition, ASO titer was normal in this patient.
With this case, we add to the clinical spectrum of ophthalmological complications in patients with IE. It is important for clinicians to accurately diagnose and differentiate between uveitis and endophthalmitis as the treatments for the two diseases are quite different. Ophthalmologic examination should be performed in patients with suspected IE. Posterior sub-Tenon triamcinolone injection could be considered in a patient who has bilateral uveitis and optic disc swelling in order to avoid the complications of systemic steroid medication.
Acknowledgements
This study was supported by a grant from the Korea Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (A111345).
Notes
No potential conflict of interest relevant to this article was reported.