 |
 |
| Korean J Ophthalmol > Volume 21(2); 2007 > Article |
Abstract
Purpose
To investigate the efficacy of lacrimal silicone intubation for the management of epiphora in patients who have previously undergone anatomically successful dacryocystorhinostomy (DCR).
Methods
The authors recruited 13 patients (4 male, 9 female) who had persistent epiphora after an anatomically successful primary external DCR and conducted lacrimal silicone intubation through the dacryocystorhinostomy site.
External dacryocystorhinostomy (DCR) is an effective surgical treatment for nasolacrimal duct obstruction, and consistently yields a success rate greater than 90%.1,2 However, epiphora might remain in some patients even after anatomically successful DCR.3,4 Moreover, as far as we are aware, no effective means of treating these functional failures has been reported.
Our interest in this topic arose when one of our patients underwent primary external DCR and silicone intubation, which successfully resolved epiphora postoperatively, but which recurred after the silicone tube was removed at 4 months postoperatively, as had been planned. The authors relocated the silicone tube in this patient, which again resolved the epiphora. This experience suggested that silicone tubes intubated into DCR sites might play a significant role in lacrimal drainage, even when a patent bypass route has been established by DCR. The authors therefore considered that silicone intubation might resolve epiphora in cases of anatomically patent but functionally failed DCR. Thus, we began to more confidently utilize this technique of silicone intubation into DCR sites to address persistent or recurrent epiphora after successful DCR. This study was conducted to evaluate the efficacy of this procedure for the correction of epiphora in patients that have received an anatomically patent but functionally failed DCR.
Among patients who received primary external DCR with silicone intubation and experienced epiphora resolution, 10 patients with epiphora recurrence immediately after silicone tube removal were included in this study. We also included 3 patients who had received primary external DCR without silicone intubation and had persistent epiphora despite an anatomically patent bypass route. All of these patients had complete nasolacrimal duct (NLD) obstruction on irrigation before primary external DCR and had no obvious punctal or eyelid abnormality. For these 13 patients, silicone intubation was conducted to manage epiphora during the study period from June 2003 to August 2005. All surgeries including primary external DCR and secondary silicone intubation were preformed by one of the authors (SIK) using a standard technique at the Seoul National University Hospital.
Before the procedure, tests were performed ensuring that all patients had an increased tear lake, appropriately positioned lower punctum, fluorescein dye retention on the dye disappearance test, and completely patent lacrimal irrigation. After informed consent had been obtained, lacrimal silicone intubation was conducted through the dacryocystorhinostomy site at an outpatient clinic. The procedure commenced with nasal packing using a 1:1 mixture of epinephrine (1 mg/ml) and 4% lidocaine. A bicanalicular silicone tube was introduced into the DCR site through the upper and lower punctum and drawn out from the nasal cavity with a straight hemostat under direct visualisation. The ends of the tube were tied together with 6-0 black silk at a point where the knot could seat deeply in the nasal cavity, and then left free in the nasal cavity.
Patients were followed up at one week, one month, and then 3 monthly after silicone intubation. On every visit, patients were asked about their epiphora symptom, and examined for tear meniscus height and silicone tube status. Postoperative assessments of epiphora were based on the subjective report and the tear lake examination. No uniform dye disappearance test was conducted postoperatively.
We performed a retrospective analysis of 13 patients who underwent secondary silicone intubation during the study period after successful DCR. Charts were reviewed for age, sex, follow-up duration, resolution of epiphora, and complications. The study was approved by the institutional review board.
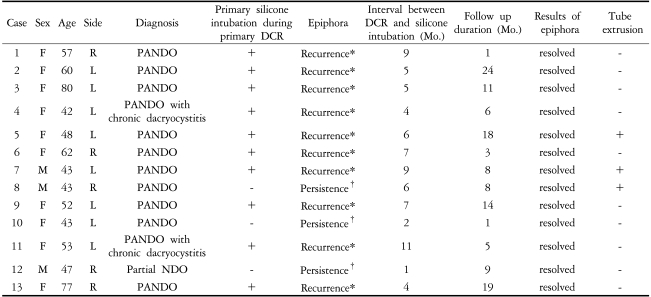
The results of secondary silicone intubation in the 13 study subjects are summarized in Table 1. Mean patient age was 54.2 years (range 42-80), mean follow-up was 13.8 months (range 6-30), and the mean interval between primary DCR and silicone intubation was 5.47 months (range 2-10). Of these 13 patients, 10 had received primary external DCR with silicone intubation and 3 had received primary external DCR without silicone intubation.
All 13 patients reported complete resolution of epiphora and presented a normal tear lake by slit lamp biomicroscopic examination after silicone intubation (Fig. 1, 2). Spontaneous tube extrusion occurred in three patients, and they complained recurrent epiphora right after its extrusion. New tubes were easily reintubated. Silicone tube-related complications, such as granuloma, canalicular or punctal slitting were absent postoperatively. As far as there is no tube-related complication, tubes will be maintained in situ.
If complete anatomic obstruction is the cause of DCR failure, a secondary bypassing surgical procedure is necessary, and may be successful.
However, in cases of failure caused by a nonfunctioning but patent DCR with no obvious punctal or eyelid abnormality, the situation is less clear. Amin et al,4 using intubation dacryocystography after DCR, found no anatomic or physiologic abnormality in 58% of patients that experienced postoperative epiphora recurrence. Furthermore, there is no known effective treatment for epiphora in cases with an anatomically patent but functionally failed DCR.
This study demonstrates that silicone intubation can result in the resolution of epiphora in cases of anatomically patent but functionally failed DCR. This approach was easily performed and proved successful in all patients. Epiphora was completely resolved in all patients, without any significant complication.
Slow dye disappearance on the fluorescein dye disappearance (FDD) test, which was observed before secondary silicone intubation in all cases of the present study, may indicate lacrimal pump dysfunction, and thus, affected patients would benefit from a procedure to augment lacrimal pump function. Therefore, we assume that lacrimal silicone intubation, conducted in the present study, must have affected the lacrimal pump.
One possible explanation why epiphora was resolved after silicone intubation is that bicanalicular silicone intubation can control punctal position by supporting it, and thus help both upper and lower puncta oppose well during the closure phase of blinking, and thus enhance lacrimal pump function. Another possible explanation is provided by the capillary phenomenon. Small canaliculi may act as capillary tubes, and capillarity tends to occur more strongly in narrow bore tubes than in wider ones. Therefore, because silicone intubation causes the canalicular lumen to narrow, it increases capillarity, and thus enhances lacrimal tear drainage. However, despite all these assumption, the exact mechanism of epiphora resolution is not clear.
We are also aware of the limitations of the present study. For example, objective postoperative lacrimal drainage assessment using the fluorescein dye disappearance test was not performed in all patients. Although these represent weaknesses in our study method, the fact that all patients improved following intervention strongly indicates that the described operative technique of silicone intubation is beneficial. We based our assessment on patients' clinical symptoms, and Schirmer testing and tear break-up time were not quantified. However, all patients presented with a complaint of tearing, were positive for dye retention on dye disappearance test, and were patent to nasolacrimal irrigation. The mean follow-up time of this study (13.8 months) is not long enough to fully evaluate long term complications by leaving the tubes in-situ indefinitely. Despite the possibility of silicone tube-related long term complications, it is still more meaningful to have silicone tube intubation and not to suffer epiphora, at least, before long-term complications may develop, than just to do nothing about the symptom for fear of complication and suffer epiphora, because there is no other established management in such cases. Moreover, it might have been beneficial, if we could assess our patients not only in a prospective fashion but if we had also looked at the nasal ostium and performed preoperative Jones 1 and 2 testing and postoperative Jones 1 testing, using nasal endoscopy, in all patients. However, as reported by Conway,5 we are in the mainstream of current ASOPRS members and do not routinely perform such testing.
Nevertheless, given the above limitations, we believe that the results obtained suggest an approach to epiphora management after anatomically successful DCR, and conclude that lacrimal silicone intubation is a simple, safe and effective procedure for patients with epiphora after anatomically successful DCR.
Notes
* Presented at American Academy of Ophthalmology Annual Meeting, October 2005; Chicago, Illinois.
REFERENCES
1. Tarbet KJ, Custer PL. External Dacryocystorhinostomy: surgical success, patient satisfaction and economic cost. Ophthalmology 1995;102:1065-1070.


2. Welham RA, Henderson PH. Results of Dacryocystorhinostomy: analysis of causes for failure. Trans Ophthalmol Soc UK 1973;93:601-609.

3. Delaney YM, Khooshabeh R. Fluorescein transit test time and symptomatic outcomes after external dacryocystorhinostomy. Ophthal Plst Reconst Surg 2002;18:281-284.

Fig.┬Ā1
Result of Fluorescein dye disappearance test before silicone intubation (A: immediately after dye instillation, B: five minutes after dye instillation) This patient complained of epiphora recurrence in the left eye after the planned removal of the silicone tube following anatomically patent DCR. Note that fluorescein dye remained in left eye on dye disappearance test (Bottom right, arrow).
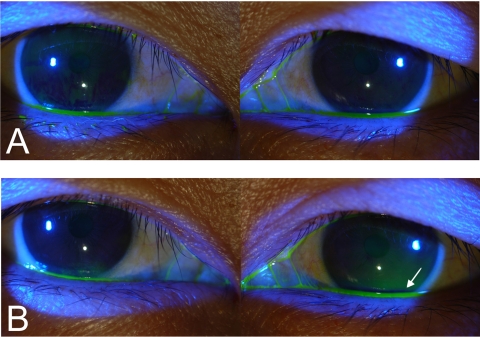
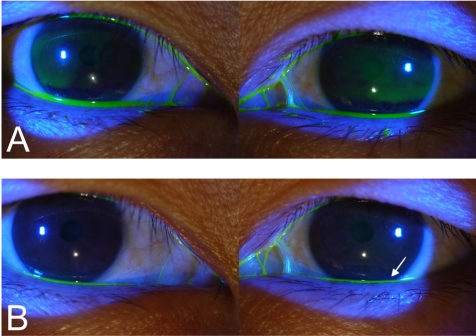
Fig.┬Ā2
Result of Fluorescein dye disappearance test of the same patient 1 month after silicone intubation in the left eye (A: immediately after dye instillation, B: five minutes after dye instillation) Note the symmetric disappearance of fluorescein dye from both eyes (Bottom right, arrow).
- TOOLS
-
METRICS

- Related articles
-
Learning Curve for Endoscopic Endonasal Dacryocystorhinostomy2017 August;31(4)



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



