 |
 |
| Korean J Ophthalmol > Volume 37(4); 2023 > Article |
|
Dear Editor,
Atypical spindle cell/pleomorphic lipomatous tumor (ASC/PLT) is a benign adipocytic neoplasm newly classified in the fifth edition of the WHO Classification of Tumors: Soft Tissue and Bone, published in 2020 [1]. Here, we report a case of ASC/PLT, which was diagnosed histopathologically, involving the orbit which is uncommon. A written informed consent for the publication of research details and clinical images was obtained from the patient.
A 57-year-old man presented with painless and progressive proptosis of the left eye that had developed 6 months earlier. The patient also complained of intermittent diplopia. He had no ocular disease or medical history.
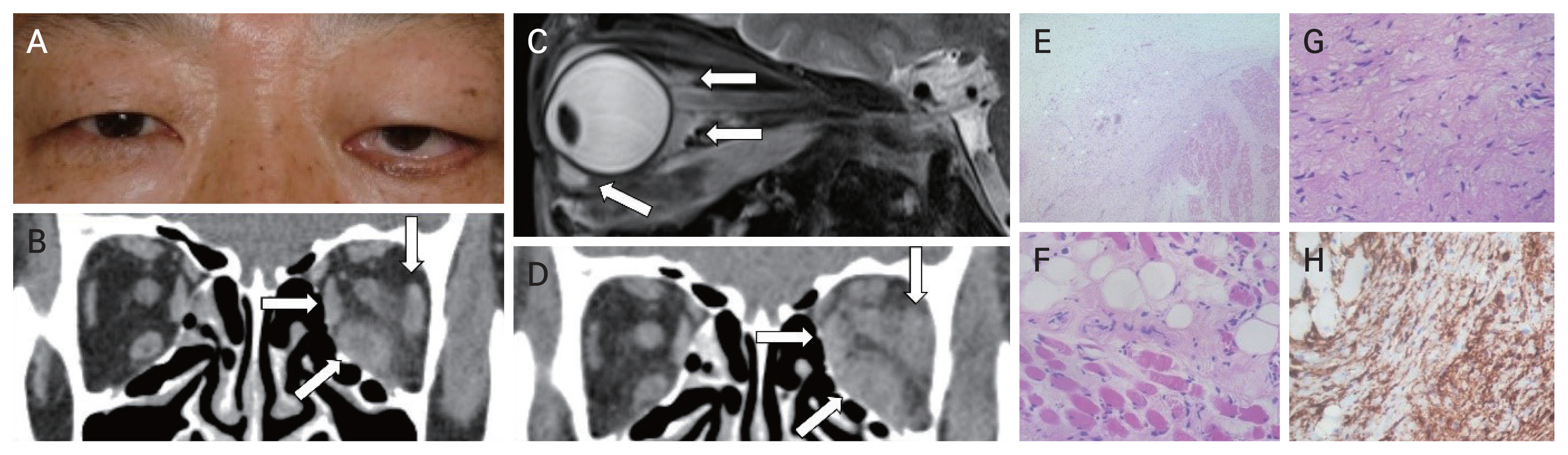
On initial evaluation, he had a best-corrected visual acuity of 25 / 20 in the right eye and 20 / 20 in the left eye, full color vision in both eyes, and no relative afferent pupillary defects. Mild lid swelling and conjunctival chemosis were present in the left eye, with no tenderness or palpable mass (Fig. 1A). Hertel exophthalmometry showed a 16-mm left eye protrusion compared to 14 mm on the right. There were −2-mm limitations to supraduction and abduction in the left eye. Fundoscopic examination results were unremarkable. Thyroid function test results were within the normal range.
Computed tomography (CT) of the orbits revealed thickening of the inferior rectus (IR), medial rectus (MR), and lateral rectus (LR) muscles of the left eye and enhancement of soft tissue in the orbit, compatible with nonspecific orbital inflammation, also known as orbital inflammatory pseudotumor and idiopathic orbital inflammation (Fig. 1B).
The patient was managed with oral prednisolone (60 mg/ day) for 3 weeks, followed by tapering for 4 weeks, but it was not effective. Orbital MRI showed severe enlargement of the IR and mild thickening of the MR and LR with hyperintensity on T2-weighted imaging, revealing extension of the infiltrating lesion into the preseptal space of the lower eyelid, which was suspected to be a lymphoma (Fig. 1C).
Three biopsies were performed in other facilities over 6 months on the demand of the patient, and a lipomatous tumor was only diagnosed on the third result. The patient returned to our hospital and was followed up for over 2 years. During this period, the patient maintained relatively good vision but complained of slightly worsening diplopia and limitation of supraduction of the left eye. Repeat CT demonstrated progression of the disease, and the decision was made to proceed with orbitotomy for the fourth biopsy to make an accurate diagnosis (Fig. 1D). All biopsies were performed from the mass infiltrating orbit (Fig. 1C). The pathology of the specimen showed that mature adipose cells were present between skeletal muscle fibers. The tumor was primarily composed of spindle cells, with some cells showing atypia. The immunohistochemical stains of MDM2 and CDK4 showed negative. A diagnosis of an ASC/PLT was confirmed (Fig. 1E-1H). The patient was sent for 3-month follow-up at another hospital on request.
A large series of 232 atypical spindle cell lipomatous tumors reported that approximately two-thirds (63%) of the tumors occur predominantly in the limbs and limb girdles, although less commonly in the head and neck, genital area, trunk, and back [2]. To the best of our knowledge, ASC/ PLT in the ocular adnexa has been previously reported in only two cases: the orbital septum and eyelid [3]. According to Ulloa-Padilla et al. [3], our tumor is differentiated from the other atypical lipomatous tumor/well-differentiated liposarcoma since MDM2 and CDK4 showed negative in immunohistochemical findings.
ASC/PLTs generally present with a slight male predominance in the fifth to sixth decades of life. This tumor is often slowly progressive and painless, consistent with the clinical course of our patient [4]. ASC/PLTs have a low recurrence rate of 10% to 15% for incompletely excised lesions. No metastasis or dedifferentiation has been documented [5]. When this patient came to our hospital, we performed a resection of the tumor as much as possible clearly differentiated from the normal tissue. Even though this tumor is benign, it could behave as locally aggressive. We recommend having a surgical margin to be maximum of the macroscopic lesion.
In conclusion, our report emphasizes the importance of accurate diagnosis in diagnostically challenging lipomatous tumors that can also involve the orbit. Further studies with various treatment modalities for ocular adnexa are warranted.
References
1. Kallen ME, Hornick JL. The 2020 WHO classification: what’s new in soft tissue tumor pathology? Am J Surg Pathol 2021;45:e1-23.

2. Marino-Enriquez A, Nascimento AF, Ligon AH, et al. Atypical spindle cell lipomatous tumor: clinicopathologic characterization of 232 cases demonstrating a morphologic spectrum. Am J Surg Pathol 2017;41:234-44.

3. Ulloa-Padilla JP, Rubio RH, Zhou S, et al. Atypical spindle cell and pleomorphic lipomatous tumor of the ocular adnexa: two cases of a rare entity. Ophthalmic Plast Reconstr Surg 2023;39:e44-9.


Fig. 1
Clinical and histopathologic findings of the orbital tumor. (A) External photograph of the patient showing proptosis, lid swelling, and conjunctival chemosis of the left eye. (B) Orbital computed tomography (CT) demonstrates thickened inferior, medial, and lateral rectus muscles of the left eye (arrows). (C) Magnetic resonance imaging shows orbital invasion of the tumor (arrows). (D) Orbital CT taken after 3 years later showed inferior, medial, and lateral rectus muscles with more thickening finding (arrows). (E-H) Histologic features of the orbital tumor. (E) At low-power field, the tumor showing infiltrative border (hematoxylin-eosin [H&E] stain, original magnification ×40). (F) Mature adipose cells are present between the skeletal muscle fibers (H&E stain, original magnification ×400). (G) At high-power field, the tumor is mainly composed of spindle cells, with some cells showing atypia (H&E stain, original magnification ×400). (H) The tumor cells showing strong positivity for CD34 staining (original magnification ×400).
- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,063 View
- 53 Download
- Related articles
-
Conjunctival Myxoid Stromal Tumor Involving Eyelid Margin: A Case Report2024 February;38(1)
Seborrheic Keratosis of the Conjunctiva: A Case Report2009 December;23(4)
Trichilemmal Carcinoma of the Upper Eyelid: A Case Report2009 December;23(4)



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



