 |
 |
| Korean J Ophthalmol > Volume 31(2); 2017 > Article |
Dear Editor,
Deposits, composed mainly of calcium-containing mixtures or inflammatory cells [1,2,3,4], may form on the surface of an intraocular lens (IOL) implanted during cataract surgery. In severe cases, a significant decrease in visual acuity may necessitate IOL replacement [1]. In this case report, we describe a patient who had refractory deposits on an IOL that spontaneously disappeared after Ahmed valve implantation was performed to control intraocular pressure (IOP).
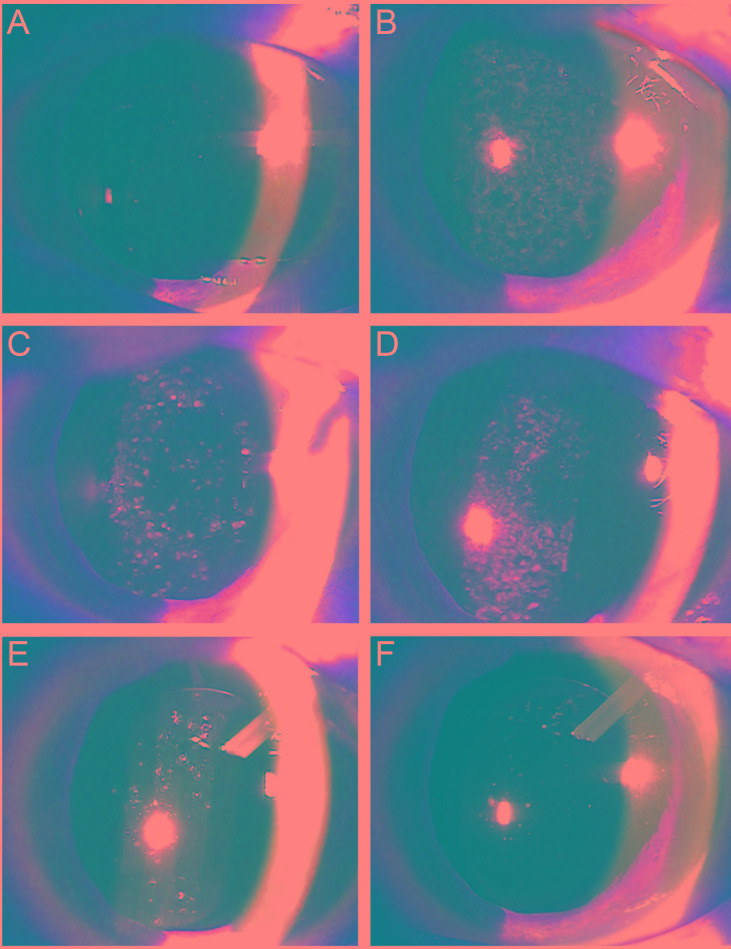
A 59-year-old male patient suffered a left traumatic cataract after a stone hit his eye while mowing grass. He was undergoing the m aximum tolerable medical t herapy for advanced primary open-angle glaucoma in both eyes. We performed vitrectomy, lensectomy, and scleral fixation with a hydrophilic acrylic IOL. Two weeks after surgery, the best-corrected visual acuity was 20 / 25 in the left eye, and the IOL was clean (Fig. 1A). At 1 month after surgery, multiple amoeboid deposits had formed on the IOL; at 6 months after surgery, the best-corrected visual acuity was reduced to 20 / 100 due to progression of deposits (Fig. 1B). He had not shown any cells or flare in the anterior chamber since 2 weeks after surgery, and there was no macular edema. The deposits were easily removed by neodymium-doped yttrium aluminium garnet (Nd:YAG) laser therapy with low-energy power (Fig. 1C), but they recurred within a few days (Fig. 1D). Two more laser treatments were performed, and these three laser treatments were combined with anti-inflammatory steroid eye drops. However, the effect was temporary.
Thirteen months after surgery, the patient underwent Ahmed valve implantation for uncontrollable wide fluctuations in IOP from 14 to 28 mmHg. Two weeks after that surgery, the IOP was controlled to <16 mmHg, and the IOL deposits decreased (Fig. 1E). Four months after surgery, almost all deposits had disappeared (Fig. 1F).
Changes in aqueous humor components are thought to be involved in the mechanism of IOL deposition. These changes occur as a result of the viscoelastic substances and/or balanced salt solution used during surgery and/or from the influx of the ointment used for eye patches immediately after surgery [3,4,5].
Park et al. [3] reported similar cases to ours, with some differences. First, in terms of pathogenesis of the IOL deposits, their cases showed anterior chamber cells. Therefore, they suggested that their cases were a type of toxic anterior segment syndrome. However, our patient had no cells or flare in the anterior chamber. Second, in terms of a therapeutic reaction, there was no recurrence of the deposition after Nd:YAG laser therapy and the combined use of steroid eye drops.
We speculated that, in our patient with glaucoma, the recurrence of deposits was caused by inefficient drainage of the aqueous humor. This possibility is consistent with the spontaneous resolution of IOL deposits after Ahmed valve implantation. In our case, it is possible that the deposits separated from the IOL by laser therapy failed to drain from the aqueous humor and then reattached to the IOL. Alternatively, a favorable environment for deposition may have been created by some components in the aqueous humor that were selectively altered by continuous dysfunction of the trabecular meshwork. If the former is the main cause of the IOL deposits, episodic care such as anterior chamber irrigation is also helpful. However, if the latter is the main cause, more invasive surgical treatment such as Ahmed valve implantation is more appropriate due to its long-lasting effect on aqueous humor drainage.
In summary, we suggest that dysfunction of the trabecular meshwork may be one of the causes of IOL deposition. Therefore, when there are IOL deposits in patients with poor aqueous humor drainage (i.e., patients with increased IOP) and the effects of laser therapy are temporary, surgical treatment to induce aqueous humor drainage may be an effective treatment option for deposition on the IOL.
REFERENCES
1. Werner L, Apple DJ, Escobar-Gomez M, et al. Postoperative deposition of calcium on the surfaces of a hydrogel intraocular lens. Ophthalmology 2000;107:2179-2185.


2. MacLean KD, Apel A, Wilson J, Werner L. Calcification of hydrophilic acrylic intraocular lenses associated with intracameral air injection following DMEK. J Cataract Refract Surg 2015;41:1310-1314.


3. Park IK, Kim JH, Kim JC, Chun YS. Nd:YAG photodisruption of toxic anterior segment syndrome related to amoeboic deposits. J Korean Ophthalmol Soc 2012;53:1334-1340.

Fig.┬Ā1
Anterior segment photographs. (A) The relatively clear intraocular lens (IOL) at postoperative 2 weeks. (B) Multiple, scattered, grayish-white deposits on the anterior and posterior surfaces of the IOL at postoperative 6 months. (C) After neodymium-doped yttrium aluminium garnet laser therapy, the IOL deposits were partially removed. (D) Gradual redeposition on the central surface of the IOL. After Ahmed valve implantation, the deposits spontaneously disappeared. (E) Two weeks after surgery. (F) Four months after surgery.
- TOOLS
-
METRICS

-
- 0 Crossref
- 0 Scopus
- 1,997 View
- 13 Download
- Related articles
-
Comparison of Accuracy of Six Modern Intraocular Lens Power Calculation Formulas2023 October;37(5)



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



