Elevation in adduction and dissociated vertical deviation (DVD) are common components of infantile strabismus. The reported prevalence of inferior oblique overaction (IOOA) and DVD ranges from 76% to 88% in infantile esotropia and 50% in infantile exotropia [
1,
2]. It was previously believed that procedures that weaken the inferior oblique muscle do not affect the DVD. In addition, it was thought that IOOA associated with DVD should be corrected with procedures of the anterior or modified anterior transposition of the inferior oblique muscle in order to maintain DVD in the primary position. Furthermore, it is thought reasonable to use this procedure in children with bilateral IOOA associated with DVD as part of the infantile strabismus complex [
3,
4].
Generally, among patients with IOOA and DVD, indication for surgery is variable. Typically, DVD appears in preschool-age and school-age children who have had horizontal muscle surgery earlier in life to correct horizontal strabismus. Currently, recommended indications for surgery include increasing frequency of manifest large DVD, associated anomalous head posture, and significant IOOA [
1,
2].
In patients with IOOA associated with DVD, the brain circuit is likely insufficient to permanently lock the eyes; hence, the average child with infantile strabismus requires at least two surgeries [
1,
2]. Therefore, if IOOA associated with DVD develops in patients with previously corrected infantile strabismus, the patient may also have poorly controlled horizontal deviation. Eso- or exodeviation may redevelop in these patients; in addition, there is a possibility that inferior oblique muscle weakening or transposition itself may affect horizontal alignment in the primary position.
This study was conducted to determine whether recurrent or consecutive horizontal deviation is a valid indication for surgery in IOOA associated with DVD and to evaluate the effects of modified bilateral inferior oblique transposition (BIOT) on horizontal deviation in the primary position.
Materials and Methods
This study followed the tenets of the Declaration of Helsinki and was approved by the institutional review board at Korea University Medical Center. A retrospective chart review was conducted on all patients with BIOT performed at Korea University Medical center from 2008 August to 2014 October. The minimum follow-up period after BIOT was more than 6 months. All patients who had prior bilateral lateral rectus (LR) or bilateral medial rectus (MR) recession to correct infantile exotropia or esotropia had recurrent or consecutive exo- and esodeviation ranging from 30 prism diopter (PD) (esotropia) to 20 PD (exotropia), and were associated with both IOOA and DVD.
Patients were excluded if they had paretic or restrictive strabismus, prior oblique muscle or vertical rectus muscle surgery, or any systemic, neurologic disorder that could affect extraocular muscle alignment.
DVD was measured using the prism and alternate cover test, with the eyes in the primary position and fixating on an accommodative target at 6 m with full refractive correction. Any concurrent horizontal deviation was initially neutralized with a horizontal prism over the contralateral eye and DVD was measured in the ipsilateral eye. The degree of IOOA was estimated from +1 to +4, according to the method described previously [
5].
One surgeon (SHK) performed all of the surgeries. As previously reported, the surgical technique of BIOT is described. The inferior oblique muscle was approached using an inferior-temporal fornix incision through the conjunctiva and Tenon's capsule. Following isolation of the inferior oblique muscle, posterior fibers of the inferior oblique muscle were bunched using one suture toward the main muscle belly. Next, the isolated inferior oblique muscle was placed onto the equator (i.e., 1 mm anterior to the equator) and was dependent on severity of DVD and IOOA such that the distal end of the inferior oblique muscle was positioned parallel to the proximal end and on a line perpendicular to the lateral corneal limbus, 0.5 mm temporal to the lateral border of the inferior rectus muscle [
6].
Correction of concurrent horizontal deviation was not performed if the horizontal deviation was less than 8 PD; however, only one female patient underwent BIOT alone even though she had 16 PD of exodeviation. For most cases, if the angle was greater than that of esodeviation or any magnitude of exodeviation, it was simultaneously corrected with MR recession or LR resection for consecutive or recurrent esotropia, LR recession or MR resection for recurrent or consecutive exotropia. The surgical magnitude of horizontal muscle was determined by the patient's angle of deviation according to standardized values [
7]. The detailed surgical method of horizontal muscle combined with BIOT is shown in
Table 1.
We divided patients into three groups: patients who had undergone BIOT alone (BIOT group), BIOT with MR recession or LR resection simultaneously (ET BIOT group), or BIOT with LR recession or MR resection simultaneously (XT BIOT group).
After surgery, all patients were observed at postoperative 1 day, 3 months, 6 months, and final visit. Preoperative horizontal deviation, postoperative horizontal deviation, degree of IOOA associated with DVD, and corrected magnitude of horizontal deviation were evaluated in each group. The corrected magnitude of horizontal deviation was calculated as the difference between preoperative horizontal deviation and horizontal deviation at the final visit.
Statistical analyses were performed using the SPSS software ver. 21.0 (IBM Corp., Armonk, NY, USA). Non-continuous variables were analyzed using the chi-square test. Kruskal-Wallis was used for the analysis of preoperative and postoperative data according to the three groups. Statistical significance was approved for p < 0.05.
Results
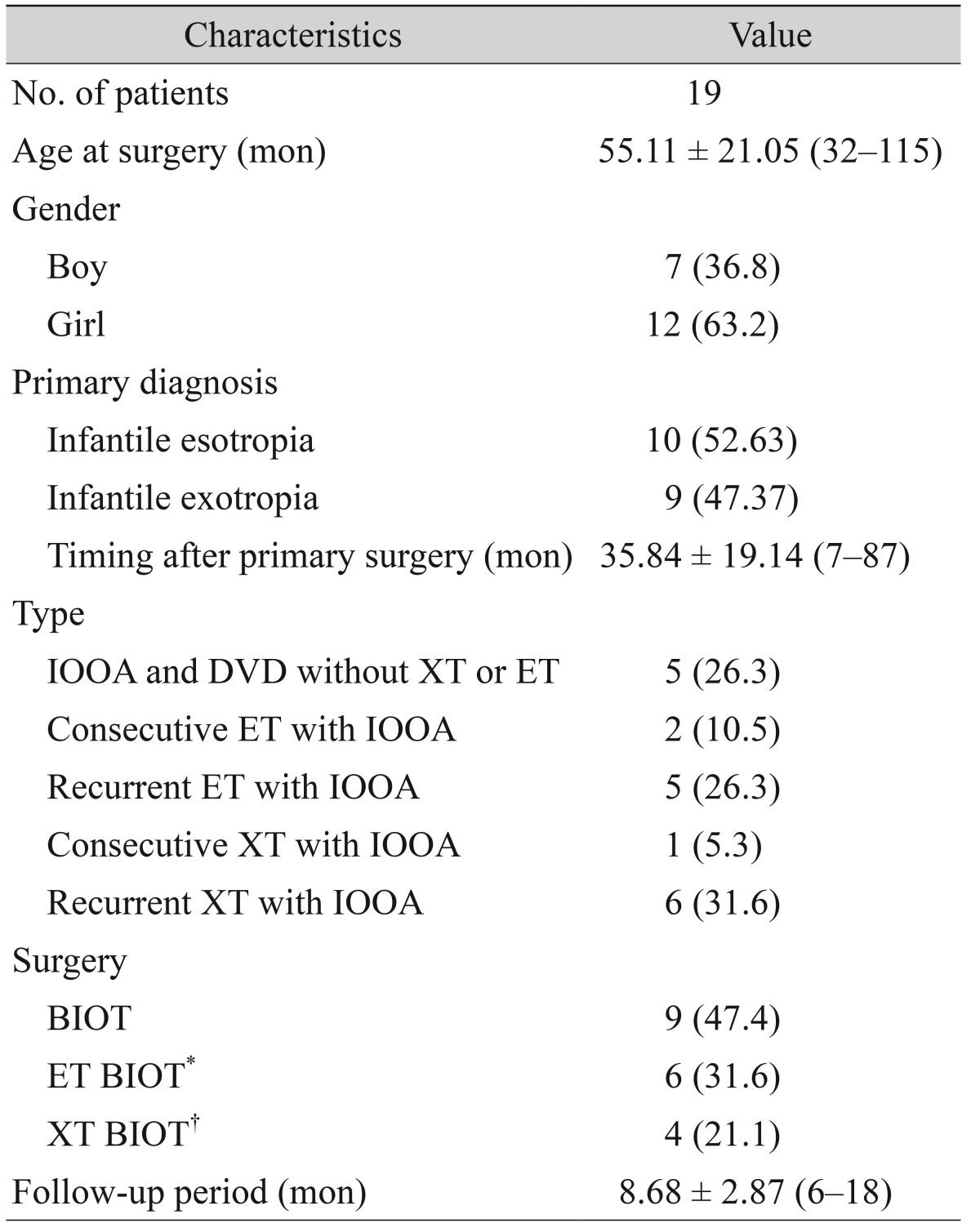
Nineteen patients were enrolled and assigned to three groups, following BIOT. The mean age at the time of surgery was 55.11 ± 21.05 months (range, 32 to 115). There were seven boys (36.8%) and 12 girls (63.2%). Mean timing after primary surgery was 35.84 ± 19.14 months (range, 7 to 87). Five patients (26.3%) had only IOOA associated with DVD without horizontal deviation. Recurrent exodeviation with IOOA associated with DVD was the most prevalent (31.6%). There were nine patients (47.4%) in the BIOT group, six patients (31.6%) in ET BIOT, and four patients (21.1%) in XT BIOT. The mean follow-up period after surgery was 8.68 ± 2.87 months (range, 6 to 18).
Table 1 summarizes the demographic characteristics.
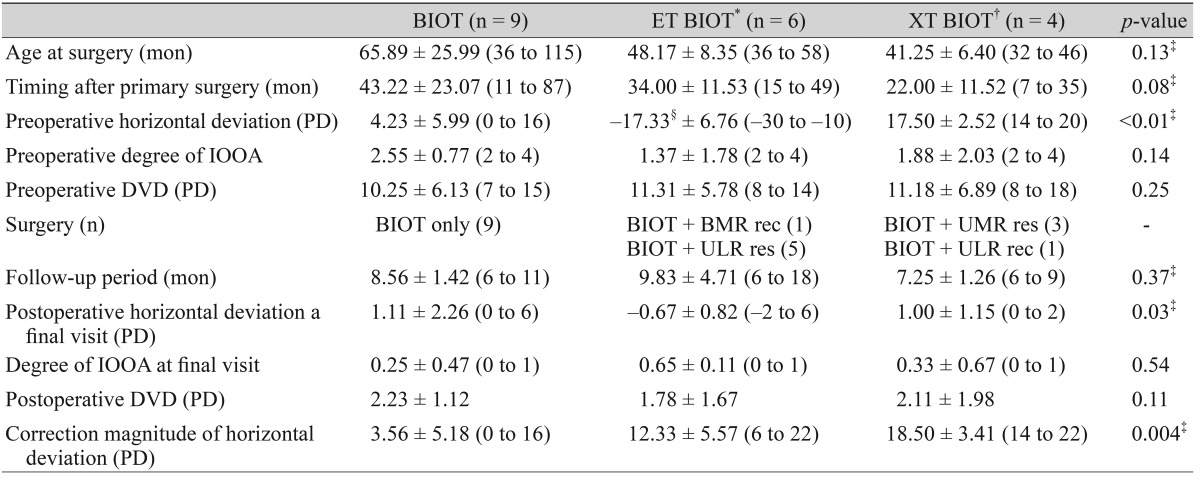
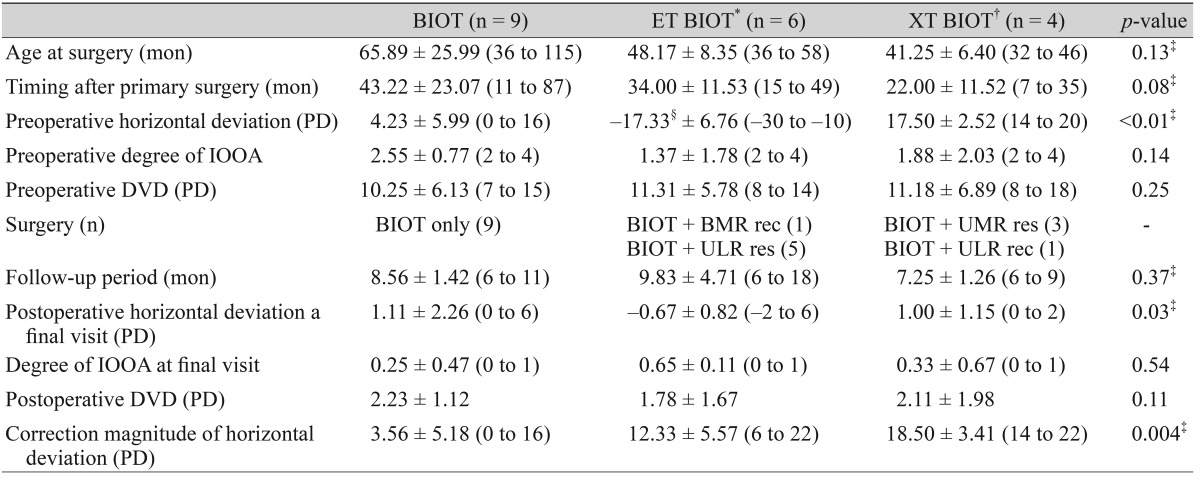
The analysis of surgical outcomes is described in
Table 2. The mean age at surgery was older (65.89 ± 25.99 months) in the BIOT group compared to other groups (48.17 ± 8.35 in ET BIOT and 41.25 ± 6.40 in XT BIOT) without statistical significance (
p = 0.13). Preoperative horizontal deviation in the BIOT, ET BIOT, and XT BIOT groups were 4.23 ± 5.99 PD (range, 0 to 16), −17.33 ± 6.76 PD (range, −30 to −10), and 17.50 ± 2.52 PD (range, 14 to 20), respectively. Esodeviation is expressed by negative values. Preoperative DVD was 10.25 ± 6.13 PD (range, 7 to 15), 11.31 ± 5.78 PD (range, 8 to 14), and 11.18 ± 6.89 PD (range, 8 to 18) in the BIOT, ET BIOT, and XT BIOT groups, respectively. Postoperative horizontal deviation at final visit was 1.11 ± 2.26 PD (range, 0 to 6) in the BIOT, −0.67 ± 0.82 PD (range, −2 to 6) in the ET BIOT, and 1.00 ± 1.15 PD (range, 0 to 2) in the XT BIOT groups. The postoperative degree of IOOA at the final visit was less than +1 in all patients. Postoperative DVD decreased to less than 5 PD in all groups (
Table 2).
Magnitude of correction in exodeviation was 3.56 ± 5.18 PD (range, 0 to 16) in BIOT and 18.50 ± 3.41 PD (range, 14 to 22) in XT BIOT groups, respectively. The corrected magnitude of esodeviation was 12.33 ± 5.57 PD (range, 6 to 22) in ET BIOT. The total horizontal deviation corrected in the XT BIOT group was significantly larger than in the ET BIOT group (p = 0.004).
Discussion
More than one surgery is often needed to achieve binocular vision and stability in infantile strabismus. Reoperation is necessary to correct residual or consecutive horizontal strabismus, oblique muscle dysfunction, DVD, or a combination of these in infantile strabismus [
8,
9]. In particular, IOOA and DVD are frequently associated with infantile esotropia after surgery [
10].
Monofixation syndrome is an eye condition defined by a small angle deviation within 8 PD and is often considered to be a stable condition in infantile strabismus. The condition of some patients will deteriorate over time with an increase in ocular deviation and loss of fusion [
11]. Uncorrected IOOA and DVD may be disruptive to the maintenance of the primary stable eye position, despite primary surgery in the early period [
12].
Whether procedures weakening the single inferior oblique muscle affect horizontal deviation has been controversial. Stager and Parks [
13] reported that in 50 patients with primary IOOA, no significant horizontal change occurred in 84% of the patients, and in 16% of those who manifested a change, it was never greater than 8 PD after bilateral inferior oblique muscle weakening alone. Wright [
5] also described that the weakening inferior oblique muscle did not significantly alter the horizontal alignment in the primary position. He suggested that when planning simultaneous horizontal and inferior oblique surgery, the magnitude of horizontal surgery should be based on measurement in the primary position, independent of inferior oblique muscle surgery. In other studies, it has been reported that the weakening of inferior oblique and superior oblique muscles resulted in esodeviation of approximately 5 to 10 PD and esodeviation of approximately 10 to 15 PD [
14]. Recently, it was reported that the median magnitude of correction of horizontal deviations with inferior oblique muscle weakening was 4 PD; however, this was variable and ranged from 0 to 20. These results are in accordance with the results from our study [
15]. Our study revealed that exodeviation (3.56 ± 5.18 PD) on average was corrected by BIOT alone. Theoretically, minimal esoshift after BIOT is due to decreasing tertiary action of inferior oblique muscles that is abducted from the primary position [
16]. In the case of prior horizontal muscle surgery, the binocular status of the patients may have an effect that requires future study. In this study, in patients with minimal exodeviation (3.56 ± 5.18 PD) associated with IOOA and DVD in infantile strabismus, BIOT alone corrected exodeviation associated with IOOA and DVD.
However, our study showed that in patients with recurrent or consecutive esotropia associated with IOOA and DVD, it is possible to obtain favorable surgical results by additional esotropia surgery such as MR recession or LR resection, as BIOT alone might aggravate esodeviation. The results of our study correspond with a recent report by Isaac and Chalita [
17] that showed patients who had undergone oblique weakening surgery in combination with MR recession might require larger MR recession to correct the primary esodeviation. On the other hand, in patients with recurrent or consecutive exodeviation associated with IOOA and DVD, BIOT alone or exotropia surgery (such as MR resection or LR recession) should be performed as appropriate, according to the magnitude of exodeviation.
Our study has limitations. First, this study was retrospective in design. Second, a small number of patients were recruited. However, currently, infantile strabismus (eso- and exo-) associated with DVD or IOOA is not a common disease. In addition, among these patients, recurrent or overcorrected esotropia is relatively rare. Further studies conducted among a large number of patients are needed. Third, mean follow-up periods after surgery were relatively short, so further long-term follow-up is needed to determine postoperative results.
In conclusion, uncorrected IOOA associated with DVD in infantile strabismus may be disruptive to the maintenance of the stable alignment after primary surgery. This condition was a valid surgical indication for BIOT. Minimal exodeviation was corrected by BIOT alone. In addition, secondary eso- or exodeviation at greater magnitudes should be corrected with proper horizontal muscle surgery along with BIOT.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
REFERENCES
1. Kraft SP. Infantile exotropia. In: Rosenbaum AL, Santiago AP, Clinical strabismus management: principles and surgical techniques. Philadelphia: W.B. Saunders; 1999. p. 176-181.
2. Tychsen L. Infantile esotropia: current neurophysiologic concepts. In: Rosenbaum AL, Santiago AP, Clinical strabismus management: principles and surgical techniques. Philadelphia: W.B. Saunders; 1999. p. 117-138.
3. Kushner BJ. Restriction of elevation in abduction after inferior oblique anteriorization.
J AAPOS 1997;1:55-62.


4. Mims JL 3rd, Wood RC. Antielevation syndrome after bilateral anterior transposition of the inferior oblique muscles: incidence and prevention.
J AAPOS 1999;3:333-336.


5. In: Wright KW, Color atlas of strabismus surgery: strategies and techniques. 3rd ed. New York: Springer; 2007. p. 136.
6. Kim SH, Na JH, Cho YA. Inferior oblique transposition onto the equator: the role of the equator in development of contralateral inferior oblique overaction.
J Pediatr Ophthalmol Strabismus 2012;49:98-102.


7. In: Wright KW, Color atlas of strabismus surgery: strategies and techniques. 3rd ed. New York: Springer; 2007. p. 191.
8. Hiles DA, Biglan AW. Early surgery of infantile exotropia.
Trans Pa Acad Ophthalmol Otolaryngol 1983;36:161-168.

9. Rubin SE, Nelson LB, Wagner RS, et al. Infantile exotropia in healthy children.
Ophthalmic Surg 1988;19:792-794.


10. Yoo EJ, Kim SH. Modified inferior oblique transposition considering the equator for primary inferior oblique overaction (IOOA) associated with dissociated vertical deviation (DVD).
Strabismus 2014;22:13-17.


11. Parks MM. The monofixation syndrome.
Trans Am Ophthalmol Soc 1969;67:609-657.


12. Tychsen L. Why do humans develop strabismus?. In: Hoyt CS, Taylor D, Pediatric ophthalmology and strabismus. 4th ed. New York: Elsevier Saunders; 2013. p. 756-763.
13. Stager DR, Parks MM. Inferior oblique weakening procedures: effect on primary position horizontal alignment.
Arch Ophthalmol 1973;90:15-16.


14. Diamond GR, Parks MM. The effect of superior oblique weakening procedures on primary position horizontal alignment.
J Pediatr Ophthalmol Strabismus 1981;18:35-38.

15. Taylan Sekeroglu H, Dikmetas O, Sanac AS, et al. Inferior oblique muscle weakening: is it possible to quantify its effects on horizontal deviations?
J Ophthalmol 2012;2012:813085



16. In: Von Noorden GK, Campos EC, Binocular vision and ocular motility: theory and management of strabismus. 4th ed. St. Louis: Mosby; 1990. p. 55.
17. Isaac CR, Chalita MR. Effect of combining oblique muscle weakening procedures with bimedial rectus recessions on the surgical correction of esotropia.
J AAPOS 2015;19:54-56.


Table 1
Demographic characteristics
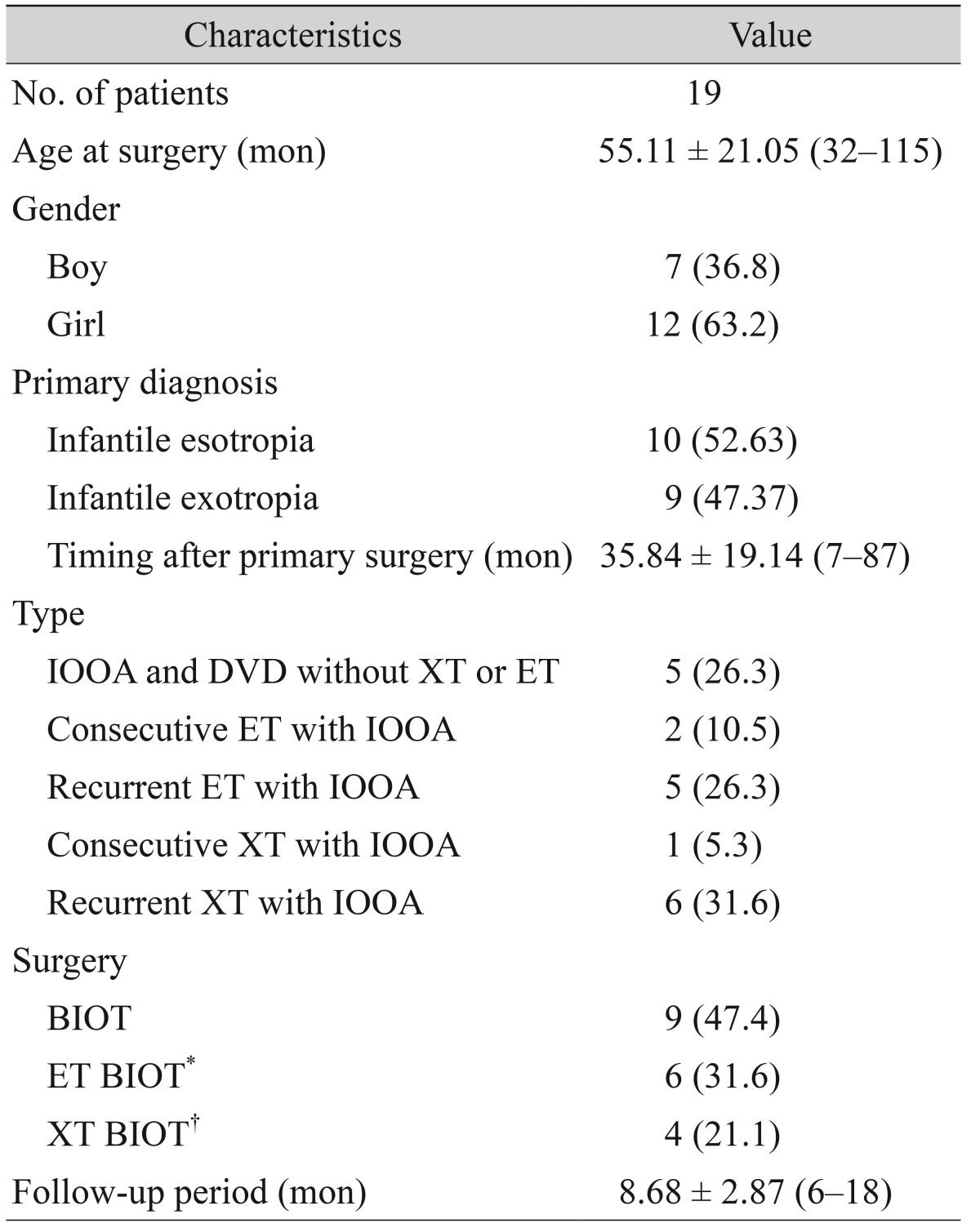
Table 2
Postoperative changes in horizontal deviation, IOOA, and DVD according to surgery






 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



