Necrotizing herpetic retinopathies have been considered a spectrum of disorders induced by herpes viruses, including cytomegalovirus (CMV); the clinical presentation of these retinopathies depends on the immune status of the patients.1
Acquired varicellar-zoster virus (VZV) retinitis produces one of two patterns of retinal involvement, each with its own characteristic clinical features. The two patterns are acute retinal necrosis syndrome and progressive outer retinal necrosis (PORN). The latter may develop in immunocompromised patients and the former typically in healthy people. Acute retinal necrosis (ARN) can be caused by the herpes simplex virus (HSV) or varicella-zoster virus (VZV).1-3 In addition, as first reported by Forster et al.4 in two patients with AIDS in 1990, rapidly progressive outer retinal necrosis may occur.3 VZV has been identified as an etiologic agent of PORN.5-9 PORN is characterized clinically as showing minimal or no inflammation in the aqueous and vitreous humors, an absence of retinal vasculitis, and patches of yellowish spots located deep in the retina. Most patients with PORN have a poor ophthalmologic prognosis, because the retinal necrosis tends to be followed by rhegmatogenous retinal detachment, and antiviral therapy with acyclovir has not been effective because of the patients' severely immunosuppressed state.10 We encountered a patient who developed the clinical picture of necrotizing herpetic retinitis suspiciously suggestive of PORN without a previous diagnosis of AIDS. When the aqueous humor was examined by PCR-RFLP, HSV type 1 (HSV-1), HSV type 2 (HSV-2), VZV, and CMV were detected. This is the first reported case of PORN accompanied by CMV infection.
Case Report
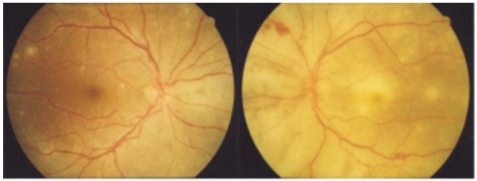
A 41-year-old Korean woman visited the ophthalmic clinic because of visual disturbance. She was determined to be a hepatitis B antigen carrier seven months prior to visiting the clinic and was treated for a mental disorder with psychiatric medication one year prior to visiting the clinic. In addition, she underwent a neck mass excision at a private clinic six months previously. A history of herpes zoster infection in the skin or elsewhere was not found. Visual acuity was 20/100 in the right eye and 20/200 in left eye. Ophthalmoscopic examination detected a deep, white outer retinal lesion in the mid-peripheral retina and posterior pole. Also, some retinal hemorrhages were noted around the major vascular arcade in the left eye (Fig. 1). Fluorescence angiography showed no active vascular leakage, but there was diffuse leakage from the subretinal area. The patient would have been referred to retinal service, but she was unreachable for one week for private reasons. When she returned to the eye clinics on June 12, 2000, her retina finding had markedly changed. The previous deep, white retinal lesions had coalesced and progressively expanded in a circumferential manner, with sparing of the perivascular retina. Retinal and vitreous hemorrhages could be noted around the optic nerve. Retinal detachment was noted at the inferior mid-periphery of the left eye. Visual acuity was 20/200 in the right eye and hand motion in the left eye (Fig. 2). Typical progressive outer retinal necrosis was considered, but would not explain the moderate retinal and vitreous hemorrhage around optic nerve. Thus, necrotizing herpetic retinopathy was considered. Intravenous treatment with acyclovir for presumed VZV or HSV retinitis was administered. A systemic work-up was evaluated, and anti-HIV antibodies and HBs Ag were detected in the serum. Anterior chamber paracentesis was taken for the identification of a specific causative agent. A 0.1 cc sample of aqueous humor was acquired for polymerase chain reaction. The PCR-RFLP analysis of the aqueous humor specimen was positive for VZV, HSV-1, HSV-2, and CMV DNA. At the same time, the patient was diagnosed with AIDS at the C3 stage (CDC classification) because of the decreased CD4+ cell count of 18 /ul and the presence of encephalopathy caused by AIDS. Because of the association between HIV infection and suspiciously combined CMV retinitis, intravenous treatment with ganciclovir was added. Forscarnet is not available in Korea. The patient was referred to Yonsei University Hospital for management of her HIV infection. After the diagnosis, she was treated with zidovudine, lamivudine, and indinavir. On June 16, in spite of medical therapy, the retinal necrosis had progressed (Fig. 3). Total retinal detachment and extensive full-thickness necrosis were found in the left eye, and inferior partial retinal and choroidal detachment were noted in the right eye. The patient's visual acuity was hand motion for both eyes.
Discussion
PORN has been reported as an acute necrotizing retinopathy caused by VZV in patients with AIDS.5 VZV antigen has been detected immunohistochemically in the outer retina in eyes showing PORN, and VZV is considered the usual etiologic agent.3 HSV-1 antigen in the peripheral retina and cytomegalic cells with positive CMV antigens in the posterior retina of CMV retinitis followed by PORN.11 Two cases of PORN in which HSV infection was suspected to be a cause have been reported.12,13 Engstrom et al.10 have retrospectively studied 65 involved eyes from 38 patients and defined the following clinical criteria for PORN: multifocal lesions characterized by deep retinal opacification without granular borders, sometimes including areas of confluent opacification; lesion location in the peripheral retina, with or without macular involvement; extremely rapid progression; absence of vascular inflammation; and minimal or no intraocular inflammation.10 PORN is further characterized by an extremely poor prognosis, as it manifests poor responses to antiviral treatment related to an immunodeficient state. Progression to the loss of light perception occurs in two-thirds of patients due to photoreceptor necrosis involving the atrophic retina. Clinically, our patient manifested multiple discrete areas of retinal opacification developed in the deep layers of each eye, concurrent with retinal and vitreous hemorrhage around the optic nerve, which are characteristics of CMV retinitis. Ophthalmic findings were characterized by the absence of intraocular inflammation, lack of retinal vasculitis, and by the rapid progression of confluent yellow-white patches corresponding to full-thickness retinal necrosis from the posterior pole to the periphery. Our patient's findings met at least four of Engstrom's criteria, with the only point of difference being that the retinal and vitreous hemorrhages initially occurred around the optic nerve.
Several reports have identified VZV as a causative agent of PORN. Herpes virus particles were detected with an electron microscope in a retinal biopsy specimen from a case of PORN, and immunohistochemical examination has demonstrated VZV antigens in the outer retina.5,7 Polymerase chain reaction (PCR) has detected VZV DNA in specimens of vitreous aspirate, surgically enucleated eye specimens, and necropsy specimens of the eye.5,6,8 Concurrent HSV-1, HSV-2, and CMV, however, have not been documented in previous reports. Anterior chamber paracentesis for PCR-RFLP showed a possible method for detecting causative agents for necrotizing retinitis. However, in our case, serum anti-CMV, anti-HSV, and anti-VZV antibodies were not detected in the serum after retinitis occurred. Therefore, serologic antibody tests may not be applicable for the detection of causative agents for retinitis in AIDS.
In our case, choroidal detachment occurred before retinal detachment, so the main inflammatory lesion in PORN might be in the choroidal layer. In addition to retinal detachment, choroidal detachment might be another final course of PORN.
For the treatment of PORN, induction doses of intravenous ganciclovir, given simultaneously with acyclovir agents, may be effective in the stabilization of the infection in some cases and to delay progression. In our case, some effects were shown to delay progression in the right eye. Based on PCR-RFLP, the causative agents could be VZV, HSV-1, HSV-2, and CMV, so a combined therapy might be more reasonable than single acyclovir therapy in treating necrotizing retinitis in AIDS patients.
In this case, retinitis was the first sign of AIDS. For this reason, we advise ophthalmologists to consider HIV infection when an unusual retinal finding with only mild or no sign of inflammation is encountered.
Although VZV has been considered the primary causative agent of PORN, we concluded that in our case, HSV-1, HSV-2, and CMV caused PORN.





 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






