 |
 |
| Korean J Ophthalmol > Volume 20(1); 2006 > Article |
Abstract
Purpose
The success rate of endoscopic dacryocystorhinostomy has been increasing with the development of better instruments and techniques. We conducted this study to evaluate the clinical results of endoscopic dacryocystorhinostomy using a Microdebrider, which has also been used for functional endoscopic sinus surgery.
Methods
We selected 76 patients (with a total of 84 affected eyes) who had been diagnosed with a nasolacrimal duct obstruction. These patients underwent an endoscopic dacryocystorhinostomy using a Microdebrider, which removed both nasal mucosa and lacrimal sac mucosa and also trimmed the margins of the ostotomy site. We assessed patients' outcomes on an anatomical basis using a dye test and endoscopy, which were used to define the anatomical success. We also arbitrarily defined functional success as whether the subjective epiphora was absent. At a four to 18 month follow-up, we monitored the clinical course to examine any recurrent episodes
Results
The symptoms were alleviated in 72 eyes, with a primary success rate of 85.7%. On nasal endoscopy, a functional failure was seen in four eyes. In these four eyes, the orifice was narrowed by the presence of either granulation tissue or conjunctivochalasis. By contrast, surgical outcomes were the anatomical failure in eight eyes. In these eight eyes, the orifice was obstructed by the presence of granulation tissue as well as the adhesion of nasal mucosa.
Dacryocystorhinostomy can be performed via a skin, intranasal, or transcanalicular approach. The first external dacryocystorhinostomy was done by Toti1 in 1904. Since then, external dacryocystorhinostomy has usually been performed because the intraoperative approach to the lacrimal sac is easy and the success rate is high. With the use of a silicone tube, the outcomes of dacryocystorhinostomy have been much improved, and the success rate has been increased to approximately 90%.
First introduced by Caldwell in 1893, an intranasal approach was attempted to perform dacryocystorhinostomy by West and Macbeth.2-4 However, this was not possible at the time because no surgical instruments existed; the surgical vision was narrow; and the approach was difficult. Accordingly, the outcomes of dacryocystorhinostomy via an intranasal approach were poor. For these reasons, dacryocystorhinostomy has been done limitedly in only cases in which the primary surgery via a skin incision was failure or the skin incision was rejected. Since then until the 1980s, dacryocystorhinostomy has been generally used by ophthalmologists, and that via a skin approach. It was also attempted via an intranasal approach by otolaryngologists, but was not established as a mainstream modality. Nevertheless, as the functional endoscopic surgery for the paranasal sinusitis has been developed since the mid-1980s, adequate surgical vision can be obtained even within the narrow intranasal cavity. The location of the lacrimal sac can be ascertained, and accurate manipulation of an endoscope is possible. Thereafter, dacryocystorhinostomy via an intranasal approach has been increasing in popularity. The success rate of dacryocystorhinostomy has been gradually increasing with both the introduction of laser therapy and the application of instruments for the nasal surgery in the 1990s.
As compared with the skin approach, an intranasal approach has many advantages. This method causes fewer incidences of tissue damage or scar tissue formation, which contributes to a better cosmetic outcome; the intranasal approach also provides easy control of nasal mucosal bleeding. Moreover, patients who undergo dacryocystorhinostomy via an intranasal approach are at a lower risk for developing intraoperative and postoperative complications, and can be fully recovered after short healing period.5 Therefore, an intranasal approach is generally preferred over a skin approach.
We performed dacryocystorhinostomy via an intranasal approach using a Microdebrider (Hummer, Storz, USA), which has been routinely used for endoscopic surgery in paranasal sinusitis. A Microdebrider allows us to effectively remove the bone and soft tissue because its rotation motor can be connected to different types of dissectors and drills. In addition, this tool enables us to obtain excellent surgical visualization because its attached aspirator absorbs the resected material along with any blood, keeping the site free of debris. Furthermore, Microdebriders help reduce adjacent tissue damage because there are refrigerants perfused within the protection tube. To enhance the success rate, the lacrimal bone must be removed in the largest piece as possible while minimizing the damage of adjacent tissue. The accurate removal of the medial lacrimal wall must also be completed. The Microdebrider has greatly improved surgeries in which it is used. The large, well-demarcated mucosa can be removed while the surgical vision is not obscured by any bleeding. There has also been a reduced operation time, a reduction in complications and an improvement in surgical outcomes.
We finally obtained results analogous to or better than the previous studies. Here, we report our results with a review of the literature.
We retrospectively reviewed the medical records of 76 patients (with a total of 84 affected eyes) who visited us with a chief complaint of epiphora between January 2002 and February 2005. These patients underwent nasolacrimal duct irrigation and dacryocystography. After this, they were diagnosed as having a lacrimal duct obstruction under the common lacrimal canaliculi, and then they underwent endoscopic dacryocystorhinostomy using a Microdebrider.
To identify anatomical anomalies or nasal diseases, we performed an intranasal examination and computed tomography (CT) preoperatively. All the surgeries were done under general anesthesia. To lower the venous pressure of the surgical site, patients' upper trunks were positioned at an approximately 15° slant. Patients' blood pressures were maintained throughout the operation to be lower than the normal value. Using wet cotton, a solution of 2% lidocaine mixed with 1:100,000 epinephrine was applied to constrict the nasal mucosa. Then, infiltration of anesthesia was done not only on the anterior side of the middle nasal concha but also on the lateral mucosa that was right and anterior to the attachment site of the middle nasal concha.
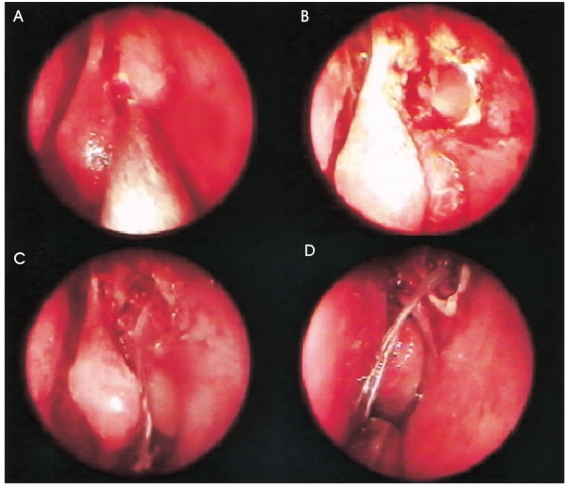
We positioned a 20-gauge light tube aimed at the posterolateral portion of the medial lacrimal sac with reference to the inferior lacrimal punctum. This light was projected to the lateral wall of the nasal cavity. Then, we located the lacrimal sac within the nasal cavity using a 4.0 mm, 0° endoscope (Hopkins rigid endoscope, Storz, USA). In the mucosa where the brightest light was emitted from the light tube, a circular incision 10 mm in diameter was made using a sickle knife. The nasal mucosa was dissected using a bone rongeur and then it was removed using an ethmoid forcep. The marginal area of mucosa was cleaned using a Microdebrider. In the medial wall of the exposed lacrimal bone and the frontal process of the maxilla, an ostium of 10 mm in diameter was made using a bone punch and a 3.0 mm microdrill. This exposed the mucosa of the lacrimal sac. The Microdebrider enables us to effectively remove the bone and soft tissue because its rotation motor can be connected to different dissectors and drills. In addition, it allows us to obtain excellent surgical visualization because its attached aspirator absorbs the resected material together with any blood. We dissected the mucosal lining the lacrimal sac and the nasal cavity using a sickle knife. Then, we were successful in dissecting the large mucosa using a Microdebrider connected to the aspirator. In removing the bone tissue (including the thick lacrimal crest), we used a microdrill as well as a Kerrison punch. We were able to make a large ostium while minimizing the damage to adjacent tissues.
By inserting a probe into the lacrimal canaliculi, we located the lacrimal sac. We made a C-shaped window in the mucosa of the lacrimal sac using a sickle knife. We removed as much of the mucosa of the lacrimal sac as possible, which had been previously incised by a Microdebrider. A silicone tube was inserted into the nasal cavity via the superior and inferior punctum. The end of the silicone tube was connected to the suction tip, and came out of the nasal cavity. Thus, a silicone tube was tightly bound on the bilateral side. The tie was then made using a 6/0 Black silk, and was positioned within the posterior nasal cavity. To prevent the formation of granulation tissue and the adhesion of new fistulae, cotton immersed in 0.4 mg/ml mitomycin C was applied to the orifice for about five minutes. Then, the orifice was rinsed using a sufficient amount of saline.
For hemostasis, a sponge pack (Merocele) (Urban and Fischer Verlag, Munich, Germany) was inserted. Postoperatively, 36-48 hours later, the sponge pack was removed. Patients were encouraged to rinse the nasal cavity on a daily basis for the first week, and thereafter to repeat the same maneuver for themselves. Patients were also encouraged to keep the silicone tube for 2-6 months (mean 13.9 weeks) while using the antibiotics and steroid eye drops. Thereafter, their use of the silicone tube was successfully weaned.
Approximately three months postoperatively, we evaluated the surgical outcomes using a dye test and nasal endoscopy. On an anatomical basis, we examined the status of the orifice and whether any granulation tissue or adhesions were present. We arbitrarily defined functional success as whether the subjective epiphora was absent. At a four to 18 month follow-up, we monitored the clinical course to examine any recurrent episodes.
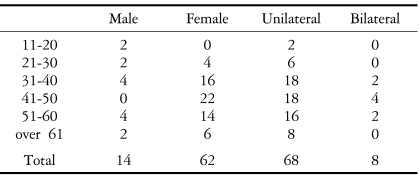
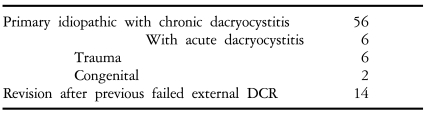
In our series, there were 14 males and 62 females which demonstrated the female predilection for this condition. Patients were between the ages of 13 and 71 years. The mean age was 45.5 years in all patients, 40.6 years in males, and 46.7 years in females (Table 1). The etiologies of nasolacrimal duct obstruction include chronic dacryocystitis due to the idiopathic obstruction of the nasolacrimal duct (56 eyes); the previous failure of dacryocystorhinostomy via a skin approach (14 eyes); acute dacryocystitis (6 eyes); trauma (6 eyes); and a congenital anomaly (2 eyes). These results are represented in Table 2.
Intraoperatively, other nasal procedures were needed in 22 eyes, which included the dissection of the anterior ethmoidal sinus (12 eyes); the dissection of the anterior middle nasal concha (6 eyes); and the correction of the nasal septum curvature (4 eyes). Otolaryngologists completed cases in which the correction of a nasal septum curvature was needed.
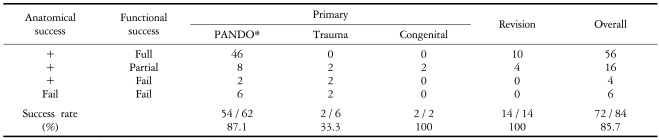
At three months postoperatively, the orifice was intact on nasal endoscopy in 84 eyes. The symptoms were alleviated in 72 eyes, and the results were very satisfactory in 56 eyes and satisfactory in 16 eyes, with a primary success rate of 85.7%. The success rate was also evaluated regarding the etiology. Of 62 idiopathic cases, 54 eyes showed excellent outcomes in which the fistula was successfully formed and the symptoms were completely or almost completely alleviated, with a success rate of 87.1%. Of six traumatic cases, however, two eyes had an improvement of symptoms with a success rate of 33.3%, which was assumed to be low. In 14 eyes in which the previous failure of dacryocystorhinostomy via a skin approach was present, the success rate was 100%. In these eyes, the surgical results were anatomically successful and the symptoms were alleviated (Table 3).
The failure of surgery was noted in 12 eyes. Upon nasal endoscopy, a functional failure was seen in four eyes. In these four eyes, the orifice was narrow and open and the epiphora was persistently present, whereas it was possible to rinse the lacrimal sac. By contrast, the surgical outcomes were an anatomical failure in eight eyes. In these eight eyes, the orifice was obstructed by the presence of granulation tissue as well as by the adhesion of the nasal mucosa. The major causes of the failure mentioned above were the complete or partial obstruction of a fistula due to the formation of granulation tissue in four eyes; the obstruction of a fistula due to the adhesion of nasal mucosa in four eyes; the obstruction of the ostium due to the regeneration of bone tissue in two eyes; and the functional epiphora due to the chronic inflammation and relaxation of palpebral conjunctiva in two eyes.
Theoretically, in a dacryocystorhinostomy through a skin incision, the suture is completed by making the graft from the nasolacrimal or nasal mucosa, and a permanent fistula can then be formed. For this reason, dacryocystorhinostomy has been favored by ophthalmologists whose success rate has been reported to be 85-99%. Nevertheless, dacryocystorhinostomy through a skin incision leaves a scar on the face and eventually leads to the development of a functional epiphora due to the scar formation or from damage to the medial canthal ligament.6 Becker7 reported that the success rate of silicone-stent insertion was 92.5% without any communications between the lacrimal sac and nasal mucosa in patients who underwent dacryocystorhinostomy via a skin approach.
The intranasal approach was widely attempted in the field of otolaryngology until the 1980s, and the success rate has been reported to be 80-90%, which is comparable to the skin approach.8,9 Nevertheless, the intranasal approach has not been established as the mainstream modality. Since the technique of endoscopic surgery for the functional paranasal sinusitis has been developed since the mid-1980s, Mcdonoch and Meiring10 first attempted dacryocystorhinostomy based on endoscopy.
Among ophthalmologists, Massaro11 first performed dacryocystorhinostomy using a laser. According to this author, an argon laser is effective in reducing the intraoperative hemorrhage, and the long-term formation of fistulas can be precipitated by the constriction of adjacent tissues. Gonnering et al.12 reported that the nasal endoscopy method was effective in obtaining good surgical vision. These authors performed a dacryocystorhinostomy using KTP and a CO2 laser. In cases in which dacryocystorhinostomy was done using only a laser, however, a large ostium cannot be formed and manipulation of the exposed lacrimal sac is difficult. This is because the internal ostium is restricted to the posteroinferior side of the lacrimal fossa. Moreover, the recurrence is predicted by the development of granulation tissue or adhesions because the high-energy laser causes damage to the lacrimal canaliculi and its adjacent tissues. Furthermore, dacryocystorhinostomy using only a laser is not effective in removing the granulation tissue or intranasal adhesions.13
Woog14 maintained that the conventional laser was not effective in removing thick anterior lacrimal crests and performing tissue biopsies from the lacrimal sac. With the combined use of the Holmium:YAG laser and surgical instruments for paransal sinusitis, these authors removed thick bone tissue using a microdrill, and also removed much of the medial wall of the lacrimal sac, reporting a success rate of 82%. Kong et al.15drew a comparison between cases in which a laser was used and those in which high-frequency surgical instruments were used to remove the nasal and lacrimal mucosa. They reported that the success rate was 67.3% in the laser group and 88.4% in the group in which high-frequency surgical instruments were used. However, these authors used an Nd:YAG laser and an otodrill to remove the thick bone tissue. In contrast, Javate16 used high-frequency surgical instruments to remove the nasal and lacrimal sac mucosa, and did a Kerrison punch to remove bone tissue; this method reported a success rate of 90%.
As described, by applying conventional instruments like a Microdebrider for the endoscopic surgery, the use of an expensive laser can be avoided, the minimal amount of tissue damage is possible, a large fistula can be formed, and the recurrence due to the formation of granulation tissue or adhesions can be prevented.
In the field of orthopedic surgery, Microdebriders have been used to remove bone or cartilage during arthroscopic surgery. In the field of otolaryngology, nasal polyps are removed and the functional surgery of paranasal sinusitis is done using a Microdebrider. Microdebriders have been reported to reduce complications and improve surgical outcomes.17,18 Unlu et al.19 reported that the obstruction of the nasolacrimal duct due to damage to the normal lacrimal sac and tract occurred during functional surgery of paranasal sinusitis. By contrast, we have postulated that the use of a Microdebrider in intranasal dacryocystorhinostomy has been effective in reducing complications and improving surgical outcomes.
A Microdebrider allows us to effectively remove the bone and soft tissue because its rotation motor can be connected to several different dissectors and drills. In addition, it enables us to obtain excellent surgical visualizaton because its attached aspirator absorbs the resected material along with blood. Furthermore, a Microdebrider reduces the damage of adjacent tissues because of the refrigerants perfused within the protection tube (Fig. 1).20 We dissected the mucosa lining the lacrimal sac and nasal cavity using a sickle knife. Then we were successful in dissecting the large mucosa using a Microdebrider connected to the aspirator. In removing the bone tissue (including the thick lacrimal crest), we used a microdrill as well as a Kerrison punch. Thus, we were able to make a large ostium while minimizing the damage to adjacent tissues.
In most cases, the failure of intranasal dacryocystorhinostomy originates from the obstruction of the fistula due to granulation tissue or the adhesion of nasal mucosa. In rare cases, the failure originates from the regeneration of the lacrimal bone, the scar formation in the lacrimal sac, the functional epiphora due to the functional insufficiency seen in elderly patients, and the obstruction of lacrimal canaliculi.
To enhance the success rate, the largest possible piece of the lacrimal bone must be removed while at the same time minimizing damage to the adjacent tissue, and the accurate removal of the medial lacrimal wall must be carried out as well. The Microdebrider reduces damage to adjacent tissues with the refrigerants that are perfused within the protection tube. This helps reduce complications and also improves surgical outcomes. Most ophthalmologists maintained that the lacrimal bone must be removed so that its diameter would be 15-20 mm. However, Linberg et al.21 reported from a long-term follow-up study that the ostium would have decreased in size until its diameter was approximately 1.8 mm. These authors maintained that the final size of the ostium was not associated with the recurrence of epiphora, and that the size of the ostium must be determined to make sure that no adjacent tissues were damaged.
Moreover, both Welham and Henderson22 and Allen et al.23 pointed out that the most likely cause of failure was the membranous obstruction. According to these authors, the membranous obstruction was due to the adhesions developed by the damage of adjacent tissues such as the nasal septum and the middle nasal concha.
The use of a Microdebrider for endoscopic surgery decreases the rate of failure; it can lessen the amount of tissue damage; a large fistula can be formed; and the recurrence due to the formation of granulation tissue or adhesions can be prevented.
There is still some controversy as to the available period for a silicone tube. According to Allen and Berlin,24 there is the possibility that a silicone tube gives rise to the surgical failure; that is, a silicone tube could irritate the adjacent tissues and thereby promote the formation of granulation tissue. However, Lee and Kim25 maintained that a silicone tube was not solely responsible for the formation of granulation tissue, but the adjuvant use of a silicone stent for enhancing the success rate of intranasal dacryocystorhinostomy increased the formation of the granulation tissue.
The maintenance period for a silicone tube was at most six months. If a silicone tube caused foreign body sensations or irritated the medial canthal angle or the mucosa adjacent to the ostium it was removed in the early stage. Finally, the overall maintenance period for a silicone tube was 13.9 weeks on average.
The advantages of intranasal dacryocystorhinostomy can be described as follows: (1) No scar tissue is formed; (2) neither the medial canthal ligament nor the angular is damaged, although these two structures were susceptible if a skin approach was used; (3) the pumping action was not hampered by the scar that formed on the lateral lacrimal wall and the adjacent muscles; (4) a differential diagnosis can be made when there are obstructions of the nasolacrimal duct due to intranasal diseases (e.g. nasal infection, allergy, the enlargement of the middle nasal concha and a defect of the nasal septum); (5) the correction of a nasal septum curvature can be coupled; and (6) acute dacryocystitis can be easily accessed, although it was not done via a skin approach.
There are several advantages to using a Microdebrider, since the large, well-demarcated mucosa can be removed because the surgeon's vision is not obstructed by any bleeding. There is also a shorter operation time, a reduction in complications and an improvement of surgical outcomes. In conclusion, the endoscopic dacryocystorhinostomy using a Microdebrider enabled us to make the large fistula while minimizing the damage to adjacent tissue. It might be the recommendable surgery to reduce complications and enhance the success rate of this procedure.
REFERENCES
1. Toti A. Nuovo metodo conservative dicura radicale delle sopourazioni croniche del sacco lacrimale (dacriocistorhinostomia). Clin Moderna 1904;10:385-387.
2. Caldwell GW. Two new operations of obstruction of the nasal duct with preservation of the canaliculi. Am J Ophthalmol 1893;10:189.
3. West M. A window resection of the nasal duct in case of stenosis. Trans Am Ophthalmol Soc 1910;12:654-658.


4. Macbeth R. Problems of lacrimal obstruction: the rhinological approach. Trans Opthal Soc U K 1956;76:355-368.
5. Lee HC, Chung WS. Success Rate of Endonasal Dacryocystorhinostomy. J Korean Ophthalmol Soc 1996;37:211-218.
6. Jones LT. Ananatomic approach to problems of the eyelids and lachrymal apparatus. Arch Ophthalmol 1961;66:111-124.


9. Berryhill BH, Dorenbusch AA. Twenty years experience with intranasal transseptal dacryocystorhinostomy. Laryngoscope 1982;92:379-381.


10. McDonogh M, Meiring JH. Endocopic transnasal dacrycystorhinostomy. J Larnygol Otol 1989;103:585-587.

11. Massaro BM, Gonnering RS, Harris GJ. Endonasal laser dacryocystorhinostomy. A new approach to nasolacrimal duct obstruction. Arch Ophthalmol 1990;108:1172-1176.


12. Gonnering RS, Lyon DB, Fisher JC. Endoscopic laserassisted lacrimal surgery. Am J Ophthalmol 1991;111:152-157.


14. Woog JJ, Metson R, Puliafito CA. Holmium:YAG endonasal laser dacryocystorhinostomy. Am J Ophthalmol 1993;116:1-10.


15. Kong YT, Kim TI, Kong BW. A report of 131 cases of endoscopic laser lacrimal surgery. Ophthalmology 1994;101:1793-1800.


16. Javate RM, Campomanes BS, Co ND, et al. The endoscope and the radiofrequency unit in DCR surgery. Ophthal Plast Reconstr Surg 1995;11:54-58.


17. Hawke WM, McCombe AW. How I do it: nasal polypectomy with an arthroscopic bone shaver: the Stryker "Hummer". J Otolaryngol 1995;24:57-59.

18. Ferguson BJ, DiBiase PA, D'Amico F. Quantitative analysis of microdebriders used in endoscopic sinus surgery. Am J Otolaryngol 1999;20:294-297.


19. Unlu HH, Goktan C, Aslan A, Tarhan S. Injury to the lacrimal apparatus after endoscopic sinus surgery: surgical implications from active transport dacryocystography. Otolaryngol Head Neck Surg 2001;124:308-312.


20. Becker DG. Technical considerations in powered instrumentation. Otolaryngol Clin North Am 1997;30:421-434.


21. Linberg JV, Anderson RL, Bumsted RM, Barreras R. Study of intranasal ostium external dacryocystorhinostomy. Arch Ophthalmol 1982;100:1758-1762.


22. Welham RA, Henderson PH. Results of dacryocystorhinostomy analysis of causes for failure. Trans Ophthalmol Soc UK 1973;93:601-609.

23. Allen KM, Berlin AJ, Levine HL. Intranasal endoscopic analysis of dacrocystorhinostomy failure. Ophthal Plast Reconstr Surg 1988;43:143-145.
24. Allen KM, Berlin AJ. Dacryocystorhinostomy failure: association with nasolacrimal silicone intubation. Ophthalmic Surg 1989;20:486-489.


25. Lee TS, Kim SW. The effects of placement of bicanalicular silicone tube and silicone stent on granuloma formation in endoscopic intranasal dacryocystorhinostomy. J Korean Ophthalmol Soc 1999;40:16-22.
Fig. 1
Microdebrider (Hummer, Storz, USA). Right: Handpiece. Left: Various cutters and protection drills.
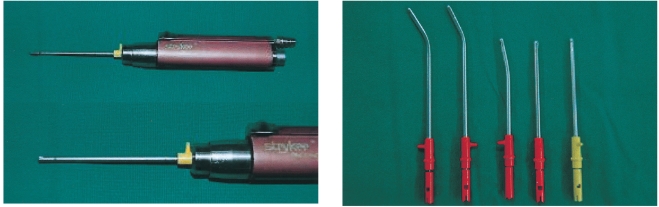
Fig. 2
(A) The nasal mucosa covering the lacrimal fossa was removed using a Microdebrider. A spot of light projected from the lacrimal sac was seen. (B) After the anterior lacrimal crest and lacrimal bone, the medial wall of the lacrimal sac was exposed. (C) The exposed medial wall of the lacrimal sac was removed by the Microdebrider. Then a bicanalicular silicone tube was inserted into the lacrimal sac through the newly formed opening. (D) One week postoperatively, the silicone tube was well-placed in the large bony opening. No damage of mucosal tissue was noted in the adjacent tissue.
- TOOLS
-
METRICS

- Related articles
-
Clinical Results of Anti-adhesion Adjuvants after Endonasal Dacryocystorhinostomy2018 December;32(6)
Learning Curve for Endoscopic Endonasal Dacryocystorhinostomy2017 August;31(4)
Effects of Nasopore Packing on Dacryocystorhinostomy2013 April;27(2)
Clinical Result of Prolonged Primary Chemotherapy in Retinoblastoma Patients.2003 June;17(1)



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



