 |
 |
| Korean J Ophthalmol > Volume 37(6); 2023 > Article |
|
Abstract
Purpose
To evaluate repeatability and agreement of chord mu between Scheimpflug tomography (Pentacam HR) and swept-source optical coherence tomography-based optical biometer (IOLMaster 700).
Methods
In this retrospective study, 63 eyes from 33 patients were included. Chord mu, X and Y Cartesian distances between the corneal vertex and the pupil center (Px and Py), and the pupil diameter were compared using two instruments. Repeatability was evaluated using intraclass correlation coefficient (ICC), coefficient of variation (CoV), and within-subject standard deviation (Sw). Interdevice agreement was evaluated using paired t-tests and Bland-Altman plots.
Results
Although Sw values for all parameters were similar between the two devices, CoV values of chord mu and pupil diameter were lower, and ICC values of those parameters were higher, in the IOLMaster 700 than in the Pentacam HR. Chord mu and pupil diameter values were higher in IOLMaster 700 than Pentacam HR (p < 0.01). The width of the 95% limit of agreement was wide for all parameters.
Conclusions
IOLMaster 700 showed better repeatability than Pentacam HR in chord mu, Px, Py, and pupil diameter values. Because there were statistically significant differences and a low level of agreement in chord mu and pupil diameter values between the two devices, they cannot be used interchangeably.
Angle kappa represents the angular difference between two lines, the visual axis (a line connecting the fovea to the fixation target) and the pupillary axis (a line connecting the corneal center to the center of the pupil) (Fig. 1A) [1]. Understanding the concept of angle kappa and its measurement is crucial for treatment planning because variation in angle kappa may affect surgical outcomes in keratorefractive and cataract surgeries [1-6]. A large angle kappa leads to a decentered ablation, which may result in undercorrection and irregular astigmatism [1,2]. A deviated multifocal intraocular lens (MFIOL) in patients with large angle kappa can also result in photic phenomena such as glare and halo and a decrease of visual acuity owing to higher order aberrations [7].
The terminology surrounding angle kappa has exhibited some ambiguity in the literature, often used interchangeably with angle lambda, which indicates the angle between the pupillary axis and line of sight (Fig. 1A). To reduce the confusion, Chang and Waring [8] introduced a novel clinical marke, chord mu, which is a two-dimensional displacement of the pupil entrance center from the subject-fixated coaxially sighted corneal light reflex, the first Purkinje reflex (P1) (Fig. 1B).
Several studies reported high repeatability of ocular parameters measured by swept-source-based optical coherence tomography (SS-OCT), IOLMaster 700 (Carl Zeiss Meditec Inc) [9,10], although there are no studies evaluating the repeatability of chord mu. In addition, agreement of the chord mu and angle kappa values between the Scheimpflug camera, Pentacam HR (Oculus) and IOLMaster 700, which are commonly used in routine cataract surgery, has not been evaluated. Therefore, the aim of this study was to investigate the repeatability and agreement of chord mu between the two devices.
The study was approved by the Institutional Review Board of the Ewha Womans University Mokdong Hospital (No. 2023-06-028) and complied with the tenets of the Declaration of Helsinki. The requirement for informed consent was waived due to the retrospective nature of the study.
This study enrolled 63 eyes from 33 patients who visited the Department of Ophthalmology, Ewha Womans University Mokdong Hospital (Seoul, Korea), between April and June 2023 for cataract surgery. Subjects who had any corneal diseases including dry eye syndrome, keratoconus, or bullous keratopathy; who had a history of retinal surgery or ocular trauma; and who used soft contact lenses within 1 week were excluded. Subjects who showed parameters with the quality label “OK” on Pentacam HR were analyzed. Measured data from IOLMaster 700 required the foveal pit to be observed on fundus OCT images to ensure good fixation and accurate measurement.
All examinations were conducted in a dark room to avoid the influence of external light in a random sequence by one experienced examiner. Prior to the measurement, the subject was instructed to blink several times, ensuring the stability of the tear film, and to gaze at the fixation target as per the manufacturer’s guidelines. Each subject underwent three measurements using both Pentacam HR and IOLMaster 700. The parameters analyzed in this study encompassed X and Y Cartesian distance (the distance between the corneal vertex and the pupil center, Px and Py), pupil diameter, and chord mu. Although IOLMaster 700 provides the chord mu value in the outcome image, Pentacam HR provides only Px and Py values. Thus, chord mu measured by Pentacam HR was calculated using the formula “r = (X2 + Y2)1/2” [11-13] (Fig. 2A, 2B). For Px, a negative value represents temporal displacement to the pupil center from the corneal vertex. Similarly, for Py, a negative value represents inferior displacements to the pupil center from the corneal vertex.
Repeatability was analyzed using the intraclass correlation coefficient (ICC), within-subject variation (Sw), and coefficient of variation (CoV). The ICC serves as an indicator of the reliability of repeated measurements, with values less than 0.5, 0.5 to less than 0.75, 0.75 to less than 0.9, and 0.90 or greater representing poor, moderate, good, and excellent reliability, respectively. Sw allows the estimation of variance. CoV was calculated by dividing the mean Sw by the average of means within subjects (CoV = Sw/mean × 100%). The CoV allows a comparison between data that have different means. A larger CoV reflects a greater level of dispersion around the mean. In this study, CoV was not calculated for X and Y coordinates because these variables can have negative values [14]. Pearson correlation coefficient values were calculated for the correlations between the two devices. A higher value indicates a stronger positive linear relationship. Interdevice comparison and agreement were evaluated using paired t-tests and Bland-Altman plots. A narrower 95% limit of agreement (LoA) indicates stronger agreement between the devices. All statistical analyses were performed using IBM SPSS ver. 26.0 (IBM Corp) and MedCalc ver. 22.009 (MedCalc Software). Statistical significance was defined as p < 0.05.
A total of 63 eyes from 33 subjects undergoing cataract surgery were included in this study. Of the patients examined, 17 were male (33 eyes, 52.4%) and 16 were female (30 eyes, 47.6%). The mean age of the participants was 67.2 ± 11.2 years (range, 29 to 84 years).
The chord mu mean was 0.26 ± 0.11 mm (range, 0.10 to 0.57 mm) when using IOLMaster 700 and 0.21 ± 0.11 mm (range, 0.04 to 0.47 mm) when using Pentacam HR (Table 1). The pupil diameter was larger when using IOLMaster 700 (3.39 ± 0.72 mm; range, 2.40 to 5.40 mm) than when using Pentacam HR (2.63 ± 0.48 mm; range, 1.89 to 3.72 mm).
Table 2 shows the mean Sw, CoV, and ICC, and the results of repeated measures analysis of variance (RMANOVA) analysis of the parameters measured using the two devices. The CoV values of chord mu and pupil diameter were higher when using Pentacam HR (26.92% and 4.75%, respectively) than when using IOLMaster 700 (14.53% and 4.39%, respectively). The ICC values of all parameters when using IOLMaster 700 were between 0.75 to 0.95, which indicated good to excellent repeatability; those of the Px, Py, and pupil diameter values when using Pentacam HR were good (0.810, 0.786, and 0.907, respectively), whereas that of the chord mu values was moderate (0.608). RMANOVA revealed that the repeated measures of all parameters in each device did not show statistical differences (p > 0.05).
When comparing the two devices, the correlation was moderate for pupil diameter (r = 0.506) and highly correlated for chord mu (r = 0.710), Px (r = 0.847), and Py (r = 0.743) (Table 3). However, there were statistically significant differences in the mean values of all parameters (p < 0.05) except for Px (p = 0.11) (Table 3). For agreement analysis, 95% LoA ranges between IOLMaster 700 and Pentacam HR were from −0.12 to 0.21 mm for chord mu, from −0.19 to 0.23 mm for Px, from −0.16 to 0.29 mm for Py, and from −0.46 to 2.00 mm for pupil diameter (Table 3 and Fig. 3A-3D).
In this study, we evaluated the repeatability and agreement of chord mu, Px, Py, and pupil diameter values between Pentacam HR and IOLMaster 700. IOLMaster 700 showed better repeatability: higher ICC in all parameters and lower CoV in chord mu and pupil diameter values compared to Pentacam HR. All parameters showed moderate to high correlation between the two devices, although there were statistically significant differences and the 95% LoA widths were wide. The different measurement method could have caused differences.
Pentacam HR uses a 360° rotating Scheimpflug camera and a 475-nm slit-light source that rotate together around the optical axes of the eye. It calculates a three-dimensional model of the anterior segment. Twenty-five images are captured within 2 seconds, with each slit image being composed of 25,000 points [15]. Pentacam HR takes 2 seconds to generate 50 sectional images, yielding in turn 138,000 distinct elevation values. Pentacam HR has a function for the screen movement of the eye. In addition to the Scheimpflug camera, there is a second frontal pupillary camera that detects and compensates for eye movement during the measuring process. Using the built-in software, eye movement is taken into consideration and the device calculates a quality specification score.
IOLMaster 700 is a noninvasive optical biometer that uses SS-OCT with a wavelength of 1,050 nm. IOLMaster 700 provides longitudinal sections of each optical interface. It determines the measurement position as the true optic axis length by imaging the fovea centralis [16]. It can take 2,000 scans/sec. It also has an alignment assistance function that ensures proper fixation by visualizing the foveal pit using a 1-mm central retina scan, thus reducing the risk of incorrect measures caused by undetected poor fixation.
Angle kappa is considered important for keratorefractive and cataract surgery outcomes [5-7]. Patients receiving diffractive or refractive types of MFIOL should exercise caution when dealing with a preoperative angle kappa exceeding 0.5 mm [2,12,17]. As a result, the measurement of angle kappa has gathered significant attention from ophthalmologists owing to its crucial importance.
The measured chord mu length or angle kappa varies in different devices. Dominguez-Vicent et al. [18] compared the angle kappa (chord mu) between Orbscan II (Orbtek, Bausch & Lomb) and Galilei G4 (Ziemer) and reported that Orbscan II measured significantly higher angle kappa values (0.43 ± 0.13 mm) than Galilei G4 (0.27 ± 0.15 mm). The authors suggested that those devices cannot be used interchangeably owing to a wide 95% LoA width (0.34 mm), in line with our results (0.33 mm). Basmak et al. [19] evaluated the angle kappa of 300 patients using synoptophore and Orbscan II, and reported that the angle kappa obtained using Orbscan II was significantly higher than that using synoptophore. The mean values of angle kappa measured using synoptophore in emmetropic eyes were 2.78 ± 0.12 for the right eye and 3.32 ± 0.13 for the left eye; those measured using Orbscan II were 5.55 ± 0.13 for the right eye and 5.62 ± 0.10 for the left eye in emmetropic eyes.
Martinez-Plaza et al. [20] assessed the repeatability and agreement of Px, Py, apparent chord mu length, and pupil diameter in static (mesopic) using Galilei G4 and dynamic (mesopic and photopic) conditions using WaveLight Topolyzer Vario (Alcon) evaluations. The study found that the repeatability of each device was very good (ICC, ≥0.89) for all parameters. When comparing the mean Px, Py, chord mu length, and pupil diameter between Topolyzer Vario on low mesopic conditions and Galilei G4 on mesopic conditions, there were significant differences in all parameters (p < 0.05). The 95% LoA widths were 0.20 mm (range, −0.01 to 0.19) for Px, 0.21 mm (range, −0.08 to 0.12) for Py, 0.24 mm (range, −0.18 to 0.06) for chord mu, and 1.45 mm (range, −3.63 to −2.18) for pupil diameter. The 95% LoA widths of every parameter were narrower than those in our study, and the authors concluded that these parameters cannot be used interchangeably. Perez-Bartolome et al. [21] compared the anterior segment SS-OCT (Anterion, Heidelberg Engineering) and Pentacam HR for corneal and pupil measurements in healthy eyes. In their study, pupil diameter and angle kappa were significantly longer when using Anterion (5.74 ± 1.34 and 0.37 ± 0.18 mm, respectively) than when using Pentacam (3.82 ± 1.60 and 0.26 ± 0.14 mm, respectively). The authors suggested that pupil diameter and chord mu values cannot be used interchangeably. To resolve the disparity in angle kappa between the devices, Yeo et al. [22] suggested a novel approach to calculate this angle using ultrasound biomicroscopy (AVISO, Quantel Medical) and Humphrey Atlas 995 (Carl Zeiss Meditec Inc) corneal topography, and compared the results with those of Orbscan II. Strong correlations and agreement were observed between the two methods, although a statistically significant disparity (p < 0.001) was observed as well.
Unlike the aforementioned studies, Qin et al. [23] compared the angle kappa in 113 patients with cataracts using Pentacam, optical low-coherence reflectometry (Lenstar LS900, Haag-Streit), and raytracing aberrometry (iTrace, Tracey Technologies), and reported that there were strong correlations and good agreement in the values between Pentacam and Lenstar LS900. However, agreements in angle kappa values were poor between Lenstar LS900 and iTrace and Pentacam and iTrace.
Holladay [24] explained the distinction between apparent chord mu (distance between P1 and the pupil center as seen through the cornea) and actual chord mu (distance unaffected by corneal magnification). In apparent chord mu, which can be measured by IOLMaster 700, the cornea magnifies the virtual image of the apparent pupil by roughly 14.0% and causes a temporal displacement of approximately 0.1 mm due to the oblique refraction. While actual chord mu, assessed by Pentacam HR, is the measurement of the visual axis to the actual pupil center. The actual chord mu changes as the frame of reference shifts from the iris lens plane to the corneal plane. In this case, the distance is smaller because it is not magnified by the cornea [24-26]. This explains the larger chord mu value measured in the IOLMaster 700 (0.26 ± 0.11 mm) compared to Pentacam HR (0.21 ± 0.11 mm) in this study.
Different pupil diameter values were also observed among devices. Qin et al. [23] evaluated the pupil diameter and reported that, unlike angle kappa, there were no differences in values among the three devices. The ICC values of intrasession reproducibility and intersession repeatability of pupil diameter were also high (ICC, >0.9). Kanellopoulos [27] compared the repeatability and agreement of indices including keratometry and pupil diameter between Pentacam HR and Orbscan II. Pentacam HR and Orbscan II showed a high repeatability of ICC (0.8 and 0.98, respectively) for pupil diameter, with no significant difference between them (p > 0.05). In contrast, Guclu et al. [28] compared parameters including pupil diameter between Pentacam HR and IOLMaster 700 in keratoconus and healthy patients and concluded that Pentacam HR and IOLMaster 700 should not be used interchangeably in normal eyes for pupil diameter, in line with our results. In their study, the mean pupil diameter of healthy eyes was 4.5 ± 1.3 mm when using Pentacam HR and 6.4 ± 1.4 mm when using IOLMaster 700. There was a statistically significant difference (1.8 ± 1.2 mm, p < 0.01) between the measurements of the two devices for healthy eyes. Rodrigues et al. [25] reported that Pentacam showed a shorter pupil diameter (3.31 mm; range, 1.87 to 5.23 mm), than the HD analyzer (5.76 mm; range, 2.50 to 8.60 mm).
Given that pupil size decreases with age [29], differences in its value between previous studies [25,28] and our study may rise from the different age of cohorts. Previous studies included younger participants (30.69 ± 7.85 years [25] and 40.3 ± 16.9 years [28]) than in our study (mean, 67.2 ± 11.2 years). In addition, the devices use different principles. Both IOLMaster 700 and Pentacam HR have alignment assistant functions; however, pupil size varies dynamically and is larger than the foveal pit (1 mm), which may have allowed a larger range of movement. These differences may also affect the differences in repeatability between the two devices.
This study has a few limitations. First, the study included subjects scheduled for cataract surgery, and thus the patients were relatively old, having the degree of cataracts that requires surgery. In addition, angle kappa may be affected by a variety of factors, such as laterality [23] and status of refraction errors [19]. Therefore, clinicians should consider these factors when applying the results of the present study in clinical practice. Second, the number of subjects was relatively small and excluded those with corneal disease such as keratoconus and bullous keratopathy, and who had a history of retinal surgery or ocular trauma. Additional studies including larger cohorts with various corneal conditions are needed.
In conclusion, IOLMaster 700 showed better repeatability than Pentacam HR in chord mu, Px, Py, and pupil diameter values. Because there were statistically significant differences and a low degree of agreement between the two devices, these parameters cannot be used interchangeably.
References
1. Hashemi H, KhabazKhoob M, Yazdani K, et al. Distribution of angle kappa measurements with Orbscan II in a population-based survey. J Refract Surg 2010;26:966-71.


2. Moshirfar M, Hoggan RN, Muthappan V. Angle kappa and its importance in refractive surgery. Oman J Ophthalmol 2013;6:151-8.



3. Fu Y, Kou J, Chen D, et al. Influence of angle kappa and angle alpha on visual quality after implantation of multifocal intraocular lenses. J Cataract Refract Surg 2019;45:1258-64.


4. Khakshoor H, McCaughey MV, Vejdani AH, et al. Use of angle kappa in myopic photorefractive keratectomy. Clin Ophthalmol 2015;9:193-5.


5. Hayashi K, Hayashi H, Nakao F, et al. Correlation between pupillary size and intraocular lens decentration and visual acuity of a zonal-progressive multifocal lens and a monofocal lens. Ophthalmology 2001;108:2011-7.


6. de Vries NE, Webers CA, Touwslager WR, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg 2011;37:859-65.


7. Harrer A, Hirnschall N, Tabernero J, et al. Variability in angle κ and its influence on higher-order aberrations in pseudophakic eyes. J Cataract Refract Surg 2017;43:1015-9.


8. Chang DH, Waring GO 4th. The subject-fixated coaxially sighted corneal light reflex: a clinical marker for centration of refractive treatments and devices. Am J Ophthalmol 2014;158:863-74.


9. Garza-Leon M, Fuentes-de la Fuente HA, Garcia-Trevino AV. Repeatability of ocular biometry with IOLMaster 700 in subjects with clear lens. Int Ophthalmol 2017;37:1133-8.



10. Michael R, Wirkner K, Engel C, et al. Feasibility and repeatability of ocular biometry measured with IOLMaster 700 in a large population-based study. Ophthalmic Physiol Opt 2023;43:860-73.


11. Park CY, Oh SY, Chuck RS. Measurement of angle kappa and centration in refractive surgery. Curr Opin Ophthalmol 2012;23:269-75.


12. Qi Y, Lin J, Leng L, et al. Role of angle κ in visual quality in patients with a trifocal diffractive intraocular lens. J Cataract Refract Surg 2018;44:949-54.


13. Narang P, Holladay J, Agarwal A, et al. Application of Purkinje images for pinhole pupilloplasty and relevance to chord length mu. J Cataract Refract Surg 2019;45:745-51.


14. Bland M. An introduction to medical statistics. 3rd ed. Oxford University Press; 2000.
15. Lackner B, Schmidinger G, Skorpik C. Validity and repeatability of anterior chamber depth measurements with Pentacam and Orbscan. Optom Vis Sci 2005;82:858-61.


16. Bullimore MA, Slade S, Yoo P, et al. An evaluation of the IOLMaster 700. Eye Contact Lens 2019;45:117-23.


17. de Vries NE, Franssen L, Webers CA, et al. Intraocular straylight after implantation of the multifocal AcrySof ReSTOR SA60D3 diffractive intraocular lens. J Cataract Refract Surg 2008;34:957-62.


18. Dominguez-Vicent A, Monsalvez-Romin D, Perez-Vives C, et al. Measurement of angle kappa with Orbscan II and Galilei G4: effect of accommodation. Graefes Arch Clin Exp Ophthalmol 2014;252:249-55.



19. Basmak H, Sahin A, Yildirim N, et al. Measurement of angle kappa with synoptophore and Orbscan II in a normal population. J Refract Surg 2007;23:456-60.


20. Martinez-Plaza E, Marcos M, Lopez-de la Rosa A, et al. Reliability and agreement of apparent chord mu measurements between static and dynamic evaluations. J Cataract Refract Surg 2023;49:21-8.


21. Perez-Bartolome F, Rocha-De-Lossada C, Sanchez-Gonzalez JM, et al. Anterior-segment swept-source ocular coherence tomography and Scheimpflug imaging agreement for keratometry and pupil measurements in healthy eyes. J Clin Med 2021;10:5789.



22. Yeo JH, Moon NJ, Lee JK. Measurement of angle kappa using ultrasound biomicroscopy and corneal topography. Korean J Ophthalmol 2017;31:257-62.




23. Qin M, Yuan Y, Wang Y, et al. Comparison of preoperative angle kappa measurements in the eyes of cataract patients obtained from Pentacam Scheimpflug system, optical low-coherence reflectometry, and ray-tracing aberrometry. BMC Ophthalmol 2022;22:153.




24. Holladay JT. Apparent chord mu and actual chord mu and their clinical value. J Cataract Refract Surg 2019;45:1198-9.


25. Rodrigues PF, Moscovici BK, Lamazales L, et al. Measurement of the visual axis through two different methods: quantification and differences for measuring chord μ. Arq Bras Oftalmol 2023 S0004-27492023005002305.

26. Rodriguez-Vallejo M, Pinero DP, Fernandez J. Avoiding misinterpretations of kappa angle for clinical research studies with Pentacam. J Optom 2019;12:71-3.



27. Kanellopoulos AJ. Scheimpflug vs scanning-slit corneal tomography: comparison of corneal and anterior chamber tomography indices for repeatability and agreement in healthy eyes. Clin Ophthalmol 2020;14:2583-92.


Fig. 1
Graphic demonstrations of ocular reference axes, angles, and chord mu. (A) Angle kappa represents the angle between pupillary axis and visual axis and angle lambda represents the angle between pupillary axis and line of sight. (B) Chord mu is the distance between corneal vertex and pupil center. Px = X Cartesian distance between corneal vertex and pupil center; Py = Y Cartesian distance between corneal vertex and pupil center.
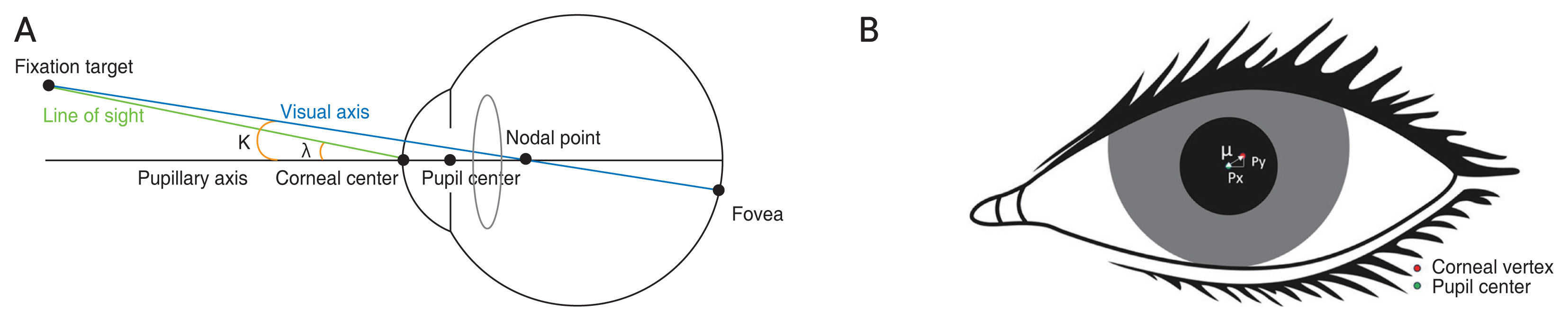
Fig. 2
Representative outcome images of pupil diameter, chord mu and X and Y Cartesian distance between corneal vertex and pupil center in (A) Pentacam HR (Oculus) and (B) IOLMaster 700 (Carl Zeiss Meditec Inc). CCT = central corneal thickness; WTW = white-to-white; Px = X Cartesian distance between corneal vertex and pupil center; Py = Y Cartesian distance between corneal vertex and pupil center.
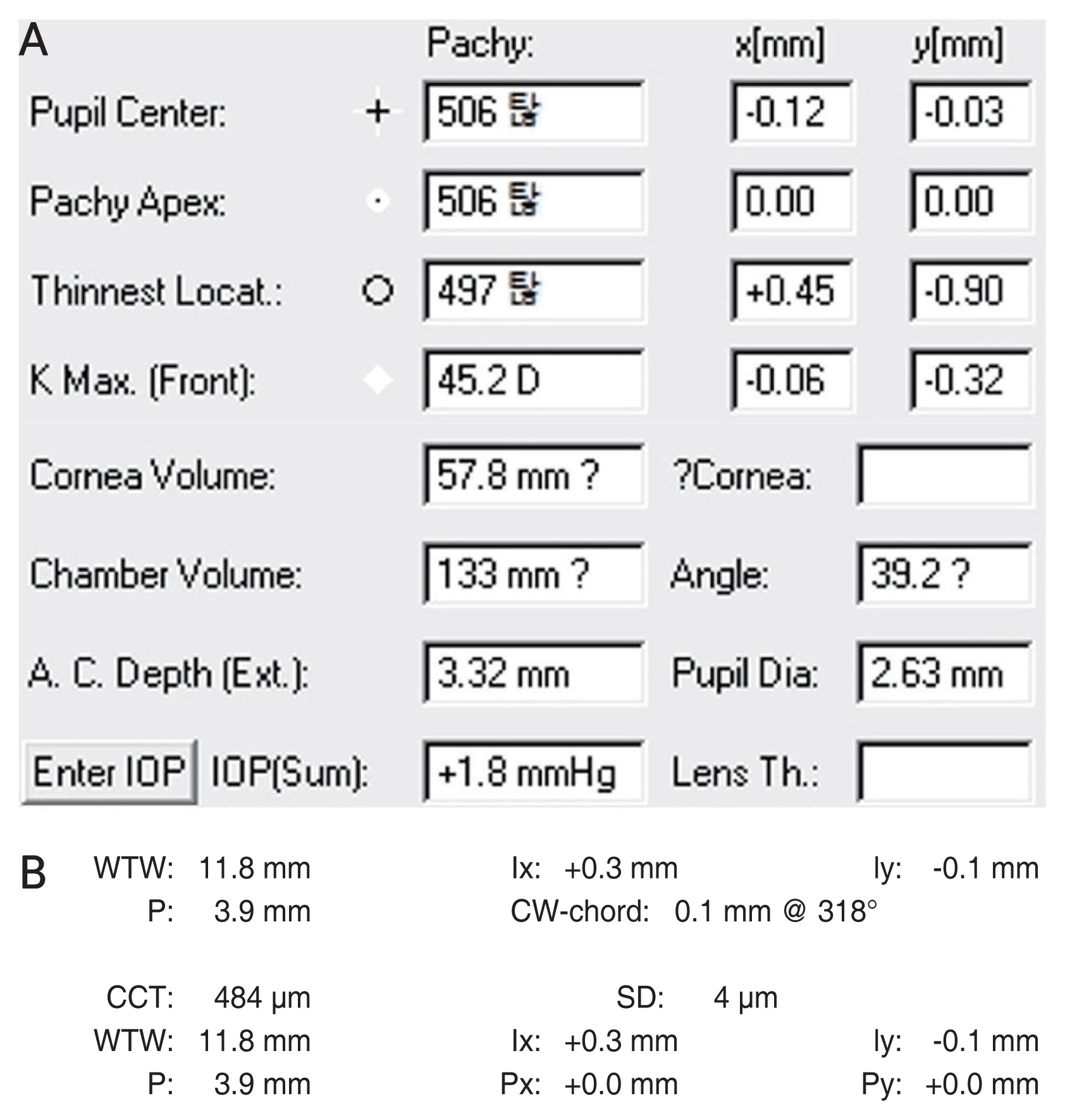
Fig. 3
The Bland-Altman plots of ocular parameters agreement between IOLMaster 700 (Carl Zeiss Meditec Inc) and Pentacam HR (Oculus). (A) Chord mu. (B) Pupil diameter. (C) X Cartesian distance between corneal vertex and pupil center (Px). (D) Y Cartesian distance between corneal vertex and pupil center (Py). SD = standard deviation.
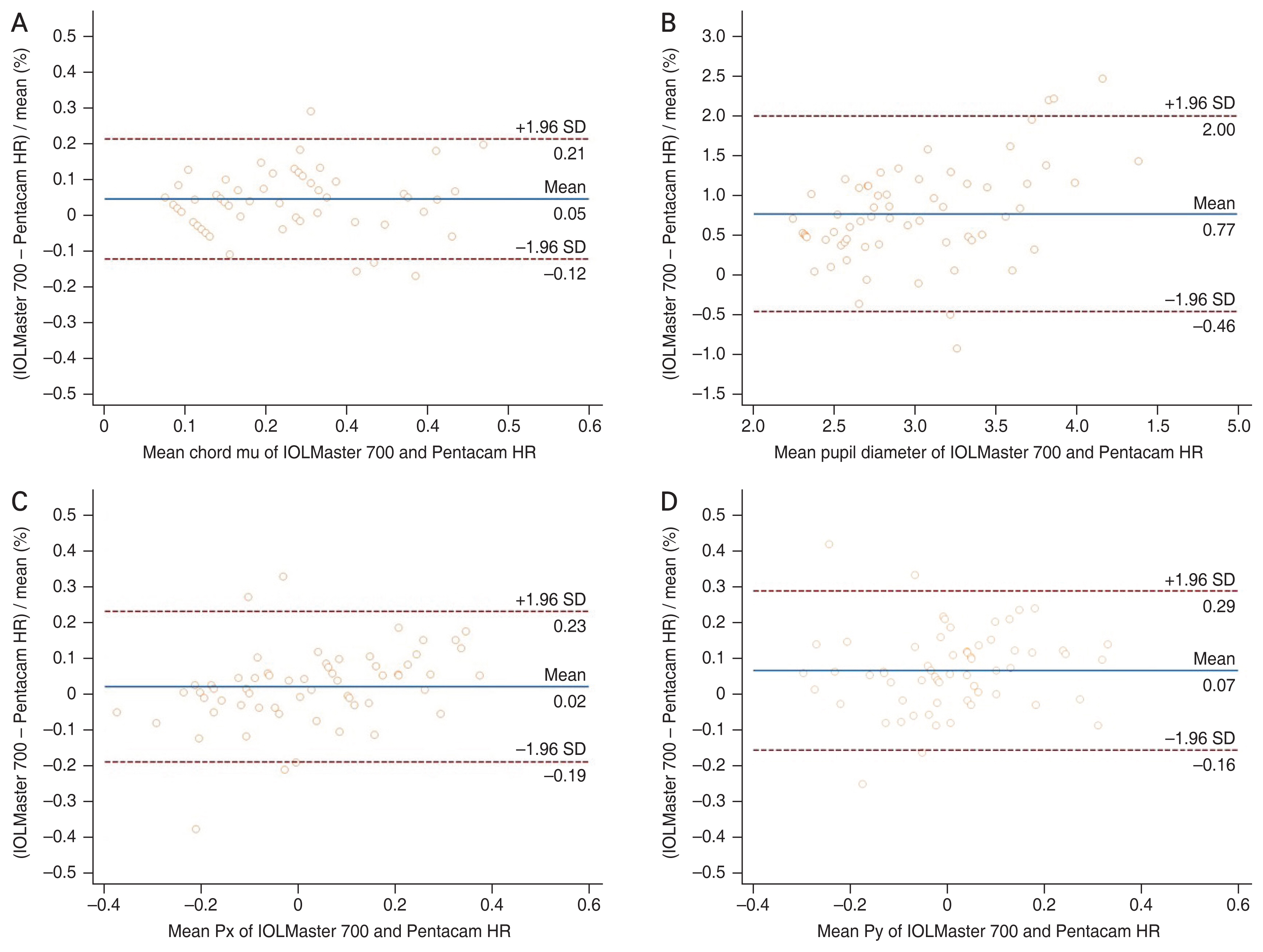
Table 1
Mean of parameters measured by IOLMaster 700 (Carl Zeiss Meditec Inc) and Pentacam HR (Oculus) (n = 63)
Table 2
Repeatability of parameters measured by IOLMaster 700 (Carl Zeiss Meditec Inc) and Pentacam HR (Oculus) (n = 63)
Sw = Within-subject standard deviation; CI = confidence interval; CoV = coefficient of variation; ICC = intraclass correlation coefficient; RMANOVA = repeated measures analysis of variance; Px = X Cartesian distance between corneal vertex and pupil center; Py = Y Cartesian distance between corneal vertex and pupil center.
Table 3
Correlation, comparison, and agreement of parameters between IOLMaster 700 (Carl Zeiss Meditec Inc) and Pentacam HR (Oculus) (n = 63)
| Parameter | Correlation coefficient* | p-value† | Paired t-test | Bland-Altman plot (95% LoA) | |
|---|---|---|---|---|---|
|
|
|||||
| t | p-value | ||||
| Chord mu (mm) | 0.710 | <0.01 | 4.227 | <0.01 | 0.33 (−0.12 to 0.21) |
| Px (mm) | 0.847 | <0.01 | 1.623 | 0.11 | 0.42 (−0.19 to 0.23) |
| Py (mm) | 0.743 | <0.01 | 4.684 | <0.01 | 0.45 (−0.16 to 0.29) |
| Pupil diameter (mm) | 0.506 | <0.01 | 9.661 | <0.01 | 2.46 (−0.46 to 2.00) |



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




