Dear Editor,
Miller Fisher syndrome (MFS) is immune-mediated peripheral neuropathy that presented with acute onset ophthalmoplegia. Ophthalmoplegia is often accompanied by ptosis. Typical clinical manifestations, such as acute diplopia with ataxia and areflexia, can make possible the diagnosis of MFS. However, atypical MFS required differential diagnosis with other neurologic diseases presented with acute ophthalmoplegia, such as ocular myasthenia gravis (OMG) [1]. OMG is a neuromuscular junction disorder and demonstrates ophthalmoplegia with ptosis. The ice test has been considered a critical step for diagnosing OMG with high sensitivity, specificity, and convenience [2]. However, previous case reports also demonstrated the positive result of the ice test beyond OMG [3,4]. We report an atypical MFS patient who had bilateral ophthalmoplegia with ptosis and a positive result to the ice test.
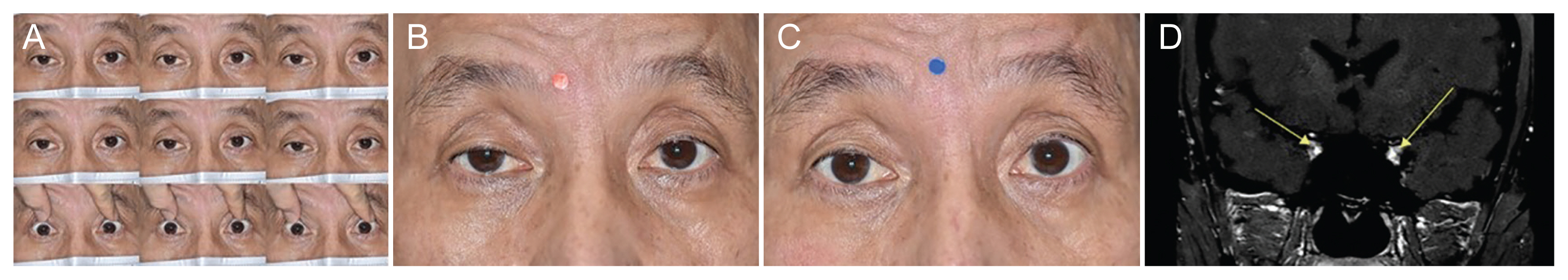
A 60-year-old male patient presented with acute bilateral ophthalmoplegia and eyelid drooping for 1 week (Fig. 1A). He complained of diarrhea and dysgeusia from 2 weeks before visiting. The ptosis was worse toward the end of the day, and ptosis in the right eye was worse than the left eye. He also complained of taste impairment and mild headache after diplopia onset. The pupils were equal, round, and no relative afferent pupillary defect. There were no significant findings on the slit lamp examination and funduscopic examination. His gait was intact and there was no areflexia. Nerve conduction studies were consistent with no definite electrophysiological evidence of peripheral neuropathy. A repetitive nerve stimulation test showed no decremental or incremental response. An ice test was performed to differential diagnosis for ptosis. The marginal reflex distance 1 increased from 0 mm to 3 mm after the ice test in the right eye, a positive result (increase ≥2 mm) (Fig. 1B, 1C). The anti-GQ1b immunoglobulin M and immunoglobulin G antibody, thyroid function test with antibodies, and anti-acetylcholine receptor antibody were within normal limits. Contrast-enhanced orbit magnetic resonance imaging showed enhancement along bilateral cranial nerve III in the cavernous sinus and orbital apex area (Fig. 1D). Although this patient had a positive result to the ice test, he was diagnosed as MFS variant due to preceding infection history, acute diplopia, and typical radiologic findings of MFS. He underwent intravenous immunoglobulin two times. There was gradual improvement in his ophthalmoplegia and ptosis within 2 months.
Ice test is a helpful screening test of OMG. It can be performed easily in clinical practice and have a high sensitivity (93%-97%) and specificity (97%-100%) [2]. The acetylcholine accumulation of the presynaptic membrane is enhanced, and the acetylcholine esterase activity is reduced, when the temperature drops. Eventually, acetylcholine is secreted more and stays in the synaptic cleft longer [2]. Even though MFS has been considered as a nerve conduction disorder, the recent experimental study demonstrated the possibility of neuromuscular junction abnormalities in the part of MFS pathophysiology [5]. We would like to suggest that the ice test can positively result in any conditions associated with neuromuscular junction dysfunction other than myasthenia gravis. The false-positive results of an ice test are rare; however, positive ice test result has been reported with orbital myositis, common pemphigus and MFS [3,4].
In our case, it was initially challenging to rule out OMG due to variation of the ptosis and positive ice tests. However, we could make a diagnosis of atypical MFS given the rapid progression of ophthalmoplegia, ptosis preceded by a diarrheal illness, and radiological findings. This patient also had a fast recovery after intravenous immunoglobulin treatment.
Ice test can be easily examined without any notable side effects, and it is useful as a screening test for myasthenia gravis due to its high sensitivity and specificity. However, as in our case, since the ice test may show a positive finding for causes other than myasthenia gravis. Therefore, we would like to suggest that it is necessary to integrate and interpret the clinical results and multimodal approaches for accurate diagnosis when the differential diagnosis is required with OMG.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






