Dear Editor,
Idiopathic orbital inflammatory syndrome (IOIS) is a nongranulomatous inflammatory process in the orbit with no known cause [1]. IOIS can cause changes such as papilledema, choroiditis, and retinal detachment [2]. Retinal vein occlusion (RVO) associated with IOIS is rare, and choroidal detachment is even rarer. We report a case of choroidal detachment and RVO with poor prognosis in IOIS that led to visual loss. Informed consent was obtained from the patient for publication of this case report and any accompanying images.
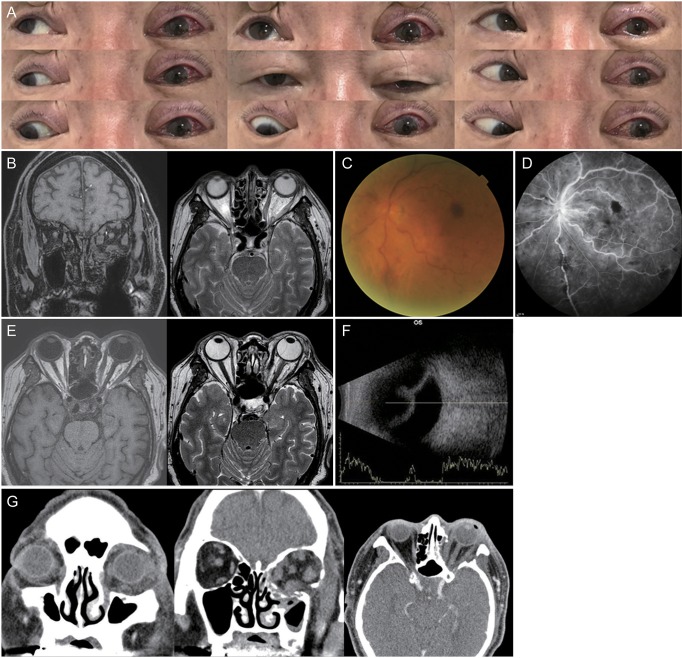
A 67-year-old man presented with a one-week history of diplopia, eyelid swelling, and exophthalmos of the left eye (OS). His medical history included diabetes and hypertension. Initial best-corrected visual acuity (BCVA) was 20 / 20 in the right eye (OD) and 20 / 25 OS, and intraocular pressure was 13 mmHg OD and 23 mmHg OS. Six prism diopters (PD) of left hypotropia in primary gaze, 20 PD of left hypertropia in downward gaze, and 12 PD of left hypotropia in upward gaze were noted. Limitation of OS was observed in all directions (Fig. 1A). Exophthalmometry read 14 mm OD and 18 mm OS. Color vision, pupil, and fundus examinations were normal. Orbital magnetic resonance imaging revealed soft tissue edema with fat infiltration in the left orbit and eyelid. Enlargement of all rectus muscles and their tendons was also observed (Fig. 1B). The superior ophthalmic vein was not enlarged in OS compared to OD, and early enhancement of the cavernous sinus was not observed. Laboratory data revealed subclinical hypothyroidism, with T3 2.07 pg/mL, free T4 0.86 ng/dL, and thyroid-stimulating hormone 27.16 mIU/L. Thyroid-stimulating hormone receptor antibody was normal. Leukocyte counts and inflammatory markers were normal, and no other sign of infection was observed. Biopsy of extraocular muscles and periorbital fat revealed degenerative hemorrhagic fibrosis with inflammation, lipoma, and microcalcification. Forced duction test revealed resistance in all directions. A diagnosis of IOIS was made, and the patient was prescribed 40 mg/day oral steroid for 3 weeks, followed by a gradual taper.
Nine weeks after the initial visit, BCVA was 20 / 200, and intraocular pressure was 18 mmHg OS. Fundus showed generalized retinal hemorrhages with tortuous veins (Fig. 1C). Fluorescein angiography revealed delayed artery-vein transit time with tortuous veins, suggesting venous congestion (Fig. 1D). The patient did not respond to steroid therapy and underwent radiotherapy.
Two weeks later, he complained of severe pain in OS. BCVA was light perception, and intraocular pressure was 27 mmHg. The light reflex was lost, and the anterior chamber became shallow. Cells were not observed, and the fundus was not visible. Newly developed fluid collection in the left suprachoroidal space was observed on magnetic resonance imaging, and choroid detachment was apparent on B-scan (Fig. 1E, 1F). For pain control and eye preservation, three-wall orbital decompression surgery was performed.
Although choroidal detachment improved postoperatively, generalized nonperfusion of the choroid and retina was observed, and optic disc pallor developed, resulting in no light perception (Fig. 1G).
IOIS typically presents with acute pain, exophthalmos, and periorbital edema. Extraocular muscle motility restrictions, ptosis, and vision loss from compression or perineuritis of the optic nerve may also be observed. Our case is a unique presentation of IOIS manifested as orbital myositis accompanied by RVO and choroidal detachment.
Several cases of IOIS-associated RVO have been reported. Though most cases showed improvement after steroid treatment, immunosuppressive treatment was needed in one case since there was no effect on both steroids and radiotherapy [3]. One case of IOIS-associated choroidal detachment accompanied by serous retinal detachment has been reported, and the patient's ocular symptoms and signs resolved in 5 weeks, and the retinal detachment resolved in 3.5 months after oral steroid treatment [4].
In our case, RVO occurred in relation to IOIS, followed by choroidal detachment without retinal detachment. Orbital edema caused by inflammation may compress orbital structures and increase resistance in retinal veins, leading to vein congestion and occlusion. Elevated venous pressure may increase colloid leakage into the suprachoroidal space, and increased vascular permeability and decreased venous outflow may cause choroidal detachment [5]. Our patient did not respond to steroid or radiation therapy, and although immunosuppressive treatment was not performed, orbital decompression surgery did not improve retinal vein occlusion.
Orbital inflammation and edema may cause choroidal detachment and retinal vein congestion in IOIS, which may lead to visual loss. Therefore, careful observation is required.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






