Pseudohypopyon after Management of Posterior Capsule Rupture Using Intracameral Triamcinolone Injection in Cataract Surgery
Article information
Dear Editor,
Rupture of the posterior capsule and prolapse of the vitreous body are relatively common complications of cataract surgery. When posterior capsule rupture (PCR) occurs, the vitreous body prolapsed into anterior chamber should be removed completely. However, the surgical procedure to remove the vitreous body is difficult and troublesome because the vitreous structure is transparent under an operating microscope and has sticky and amorphous characteristics.
Triamcinolone acetonide (TA) has been used to visualize the vitreous body prolapsed into the anterior chamber after PCR during cataract surgery [1]. Occasionally, following an intracameral or intravitreal injection, TA particles may migrate into the anterior chamber, lay in the inferior angle, and form a pseudohypopyon [2]. We present a patient who developed a pseudohypopyon following intracameral TA injection for the verification of prolapsed vitreous body during management of PCR in cataract surgery.
A 57-year-old, healthy, woman presented with decreased vision in her left eye. She was diagnosed with age-related left cataract and scheduled for cataract operation. Under topical anesthesia, standard phacoemulsification was performed in the operating room. When the posterior capsule was ruptured and the vitreous body was prolapsed into the anterior chamber, anterior vitrectomy was done to remove the prolapsed vitreous. TA solution (4 mg/0.1 mL) was injected at the location where the vitreous body was likely to have been placed using a syringe with a dull-edged needle. Immediately, the prolapsed vitreous appeared as a white-colored gel. Then, vitreous with TA granules was easily removed with a vitreous cutter. After removing the prolapsed vitreous, an intraocular lens was inserted by using sulcus fixation. At the end of operation, TA was clearly eliminated from the anterior chamber and anterior vitreous cavity. On the 1st day postoperatively, she was noted to have 3 × 4-mm sized yellow-whitish deposits in the inferior portion of the anterior chamber (Fig. 1). The visual acuity of her left eye was finger counting at 30 cm. She did not report any pain, redness or lid edema. Only topical antibiotic was applied, and the patient was followed-up on a weekly basis. The yellow-whitish deposits in the anterior chamber cleared spontaneously on the 5th week postoperatively. The visual acuity of her left eye was improved to 20 / 20 without any specific complications or treatments.
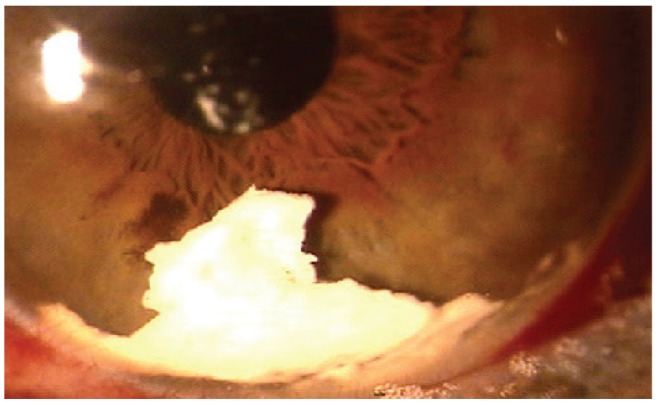
Yellow-whitish deposits seen in the anterior chamber 1 day following cataract surgery with triamcinolone acetonide for visualizing prolapsed vitreous body due to posterior capsule rupture. Some triamcinolone acetonide particles were seen on the intraocular lens surface.
Although intracameral and intravitreal TA is widely used in anterior or posterior vitrectomy to help visualize the vitreous body, it is associated with the potential risk of developing postoperative complications including endophthalmitis and intraocular pressure elevation. However, in this case, endophthalmitis was not observed; instead we observed a TA-related pseudohypopyon. The pseudohypopyon can be explained due to the passage of remnant TA from the vitreous cavity to the anterior chamber as a result of eye movements. Another theory which explains this condition is an aseptic inflammatory reaction against the excipient of the TA [3].
The development of endophthalmitis following intracameral or intravitreal TA injection must be ruled out when a pseudohypopyon is present. Usually a pseudohypopyon is distinguishable from an infective hypopyon by its ground glass appearance, the presence of refractile particles, and its shifting position, which is dependent upon the patient's head position. The presence of other associated clinical symptoms and signs may help to establish the correct diagnosis.
In conclusion, we report a case of pseudohypopyon after intracameral TA injection for the verification of remnant vitreous during the management of PCR in phacoemulsification and intraocular lens insertion, from which the patient completely recovered without any specific treatment. However, care should be taken that pseudohypopyon are distinguished from endophthalmitis and any other pathologic conditions after anterior vitrectomies with TA in cataract surgery.
Notes
No potential conflict of interest relevant to this article was reported.