Dear Editor,
Micropulse transscleral cyclophotocoagulation (MP-TSCPC) as a treatment for glaucoma patients has been elucidated for the effectiveness and safety of the procedure. By delivering energy “pulse” with resting periods, the adjacent tissues are less injured and the rate of complication lower compared to the conventional transscleral cyclophotocoagulation. Neurotrophic keratopathy (NK) is a serious complication that can impair vision. NK after MP-TSCPC is a rare complication and has been only reported in patients with diabetes mellitus (DM). In this article, we report a case of NK after MP-TSCPC in a patient without underlying diseases such as DM.
A 81-year-old Korean male with no history of DM was referred to our clinic for poorly controlled intraocular pressure (IOP) despite maximal medical therapy due to pseudoexfoliation glaucoma. He had no history of laser treatment or intraocular surgery except for uncomplicated cataract surgery and was on topical dorzolamide/timolol combination, brimonidine and bimatoprost. His visual acuity was 20 / 20 in right eye and 20 / 50 in left eye, and his IOP was 11 and 27 mmHg on the right and left eye, respectively. Slit lamp examination was notable for clear cornea and anterior chamber in both eyes with mild pigmentation in the right eye and moderate pigmentation in the left eye on gonioscopy. Optic nerve examination showed 0.7 cup-to-disc ratio and advanced cupping in the right and left eye, respectively. Visual field in the left eye showed advanced scotoma. The endothelial cell density was 1,553/mm2 and 1,232/mm2 in the right and the left eye, respectively. The patient underwent MP-TSCPC in the left eye to halt the progression of advanced disease. Cyclo G6 (Iridex Corporation, Mountain View, CA, USA) was used at 2,000 mW power with a 31.3% duty cycle, along 360 degrees for 180 seconds. The probe was seated on the conjunctiva 3 mm apart from the limbus, and was moved in a painting fashion with slight pressure along the limbus beginning at the superior half, and subsequently the remaining 180 degrees inferior half were filled in. The 3 and 9 o’clock positions were marked in a sitting position before anesthesia and were left untreated. The cornea was moistened during the procedure.
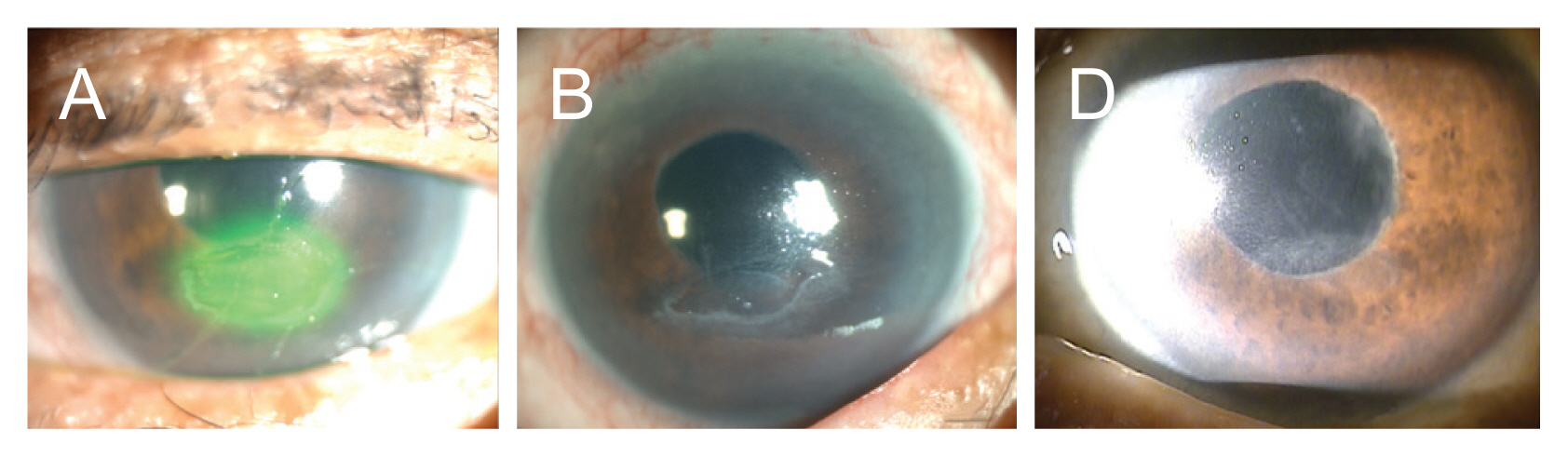
Postoperative medication included topical steroids and antibiotics, in addition to previous IOP-lowering agents. At postoperative week 1, IOP was 10 mmHg and there was a 2 × 3-mm sized painless epithelial defect in the interpalpebral region of the left cornea with heaped margins. Corneal sensation measured by Cochet-Bonnet esthesiometer was reduced in all quadrants. Bandage contact lens was applied and topical steroids and all IOP-lowering agents were discontinued. Despite the application of lubricants and topical solcoseryl concentrate, the epithelial defect persisted for 3 months, leaving a central corneal opacity (Fig. 1A-1C). Postoperative IOP ranged from 10 to 16 mmHg without glaucoma medications. At postoperative 1 year, the visual acuity was 20 / 200 in the left eye.
After MP-TSCPC, the patient showed sustained painless epithelial defect with heaped margin which is clinically coherent with NK. Previous studies reported little or no vision-threatening complications after MP-TSCPC [1]. However, Williams et al. [2] reported relatively higher rate of complications than other studies, especially in non-Caucasian race. This can be attributed to darker iris color in the non-Caucasian race than the Caucasians which increases energy absorption into adjacent tissue. Perez et al. [3] reported two cases of NK after MP-TSCPC. The patients were Asian and Hispanic, had previous history of vitrectomy and Ahmed valve implantation, and both had DM. Of note, this patient had no underlying systemic disease or previous surgical history except for uncomplicated cataract surgery. There was no observable corneal lesion at postoperative day 1, and the epithelial defect was noticed at a regular follow-up. We hypothesized that the energy absorption was high due to the dark-colored iris, and that the perilimbal nerve plexus had been thermally damaged. It might be reasonable to shorten treatment time in heavily pigmented iris. Additionally, the endothelial cell density of the treated eye was slightly decreased compared to the healthy normal range. The ability of the cornea to withstand the damage caused by the procedure might have been impaired. The operator should take cautions when performing MP-TSCPC in patients with darker iris color and lower endothelial cell density. Individualizing treatment protocols could be considered and patients should be monitored closely postoperatively.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print






