 |
 |
| Korean J Ophthalmol > Volume 30(4); 2016 > Article |
Dear Editor,
Ocular decompression retinopathy (ODR) presents as retinal hemorrhages following acute reduction of intraocular pressure (IOP) [1]. A sudden increase in retinal intravascular flow due to hypotony and defective autoregulation of blood vessels due to longstanding glaucoma consequently lead to retinal hemorrhages [2,3]. Retinal hemorrhages in ODR should be distinguished from differential diagnoses including central retinal vein occlusion (CRVO), valsalva retinopathy, and ocular ischemic syndrome, since therapies for these diseases are different. We report a case of multiple retinal hemorrhages in ODR mimicking CRVO.
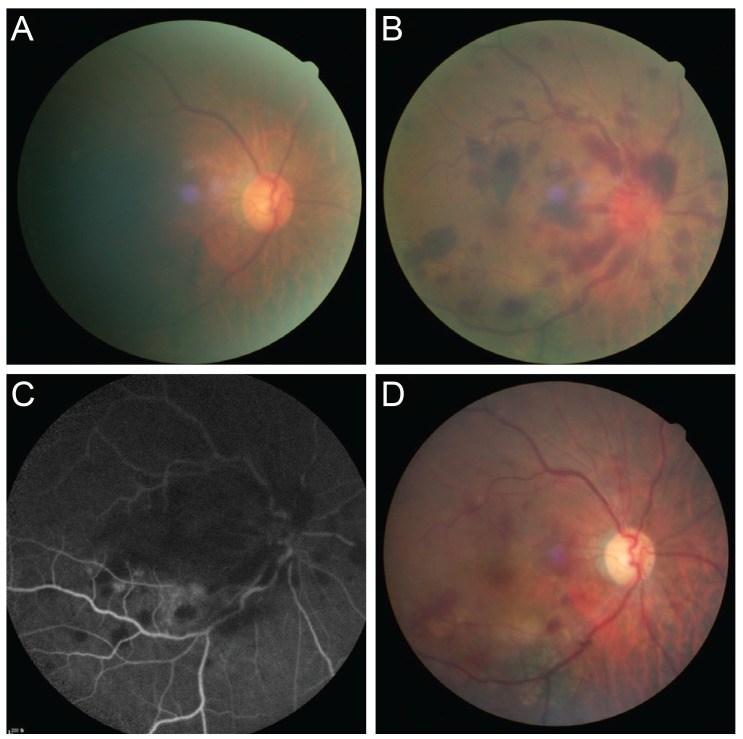
A 74-year-old female patient was referred to Daegu Fatima Hospital due to sudden ocular pain and sudden decrease in visual acuity in the right eye. Her best-corrected visual acuity was 20 / 200 in the right eye and 20 / 25 in the left eye and IOP was 68 mmHg in the right eye and 14 mmHg in the left eye. There were signs of acute angle closure including corneal edema, mildly dilated pupil, and shallow anterior chamber in the right eye. The optic discs had slight disc hyperemia in the right eye under a high IOP state (Fig. 1A). The patient was treated with intravenous mannitol 15% 250 mg, acetazolamide two tablets, and topical dorzolamide-timolol and pilocarpine 2% eye drops. After 2 hours, IOP in the right eye decreased to 24 mmHg, and visual acuity increased to 20 / 100; however, fundus exam revealed slight tortuous veins and multiple retinal hemorrhages scattered throughout the fovea, posterior pole, and peripheral retina in the right eye, similar to CRVO (Fig. 1B). Fluorescein angiography showed no delayed filling of the retinal artery or vein (Fig. 1C). After a 1-week follow-up period, her visual acuity was further decreased, and fundus exam revealed massive vitreous hemorrhage involving the fovea in the right eye. We misdiagnosed a vitreous hemorrhage and retinal hemorrhages as a presenting sign of CRVO. Two weeks later, a 23-gauge pars plana vitrectomy was performed in the right eye. One month after the surgery, the visual acuity in the right eye improved to 20 / 50, and the IOP in the right eye was 13 mmHg. Fundus exam showed reduced retinal hemorrhages and vitreous hemorrhage (Fig. 1D).
In conclusion, multiple retinal hemorrhages due to abrupt hypotony occur in ODR and can mimic CRVO. However, there are differences between ODR and CRVO [2]. Compared with CRVO, 80% of patients with ODR are asymptomatic. In clinical findings, oval-shaped hemorrhages occur in all retinal layers, and there is no severe venous dilatation or delayed venous filling on fluorescein angiography as is expected in acute CRVO. Therefore, in case of multiple retinal hemorrhages after resolution of high IOP, careful observation is required during diagnosis, and various evaluations should be carried out for differential diagnosis.
Conflicts of interest
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
Fig.┬Ā1
Fundus photographs showing the clinical course of the patient. (A) Fundus photograph of the right eye showed slight disc hyperemia. (B) Fundus photograph of the right eye showed multiple retinal hemorrhages scattered throughout the fovea and posterior pole, mimicking central retinal vein occlusion after intraocular pressure decrease. (C) Fluorescein angiography showed multiple areas of blocked fluorescence due to retinal hemorrhage and vitreous hemorrhage but no delayed venous filling. (D) One month after pars plana vitrectomy, disc hyperemia and hemorrhages were resolved.



 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




