 |
 |
| Korean J Ophthalmol > Volume 24(5); 2010 > Article |
Abstract
A previously healthy 50-year-old man was transferred to our hospital for evaluation of acute inflammation in his right eye after ocular trauma while using a grass mower. Slit lamp examination showed 1 mm-length full thickness corneal laceration without leakage, 4+ cells and inflammatory membrane in the anterior chamber, 10% hypopyon, posterior synechiae formation, and cataract change. Upon orbital computerized tomography, a metallic intraocular foreign body in the lens was indentified. Vitrectomy, phacoemulsification, foreign body removal, anterior chamber irrigation, and intravitreal antibiotics injections of vancomycin and ceftazidime were performed. In a culture of humor from the anterior chamber grew Pantoea species. More procedures were performed, including intravitreal antibiotics injection of ceftazidime. Upon administering a course of intravenous ceftazidime, fortified ceftazidime and moxifloxacin eye drops, and oral prednisolone, the patient improved.
Endophthalmitis is an uncommon but potentially devastating complication of penetrating ocular injuries with retained intraocular foreign bodies (IOFBs) [1]. Retained IOFBs are associated with endophthalmitis in approximately 6.9 to 30% of cases [2-5].
Pantoea species is a Gram-negative aerobic bacillus in the family Enterobacteriaceae. All species of the genus Pantoea can be isolated from feculent material, plants, and soil, where they can be either pathogens or commensals. Pantoea agglomerans (P. agglomerans synonyms, Erwinia herbicola, Enterobacter agglomerans) and other Pantoea species cause infections in humans and are also pathogenic to plants. P. agglomerans was most associated with penetrating trauma by vegetative material and catheter-related bacteremia [6-8].
We report a case of a patient who had endophthalmitis caused by Pantoea species infection via a retained metallic IOFB, which has not been reported previously in Korea.
A 50-year-old healthy man was transferred to our hospital for evaluation of acute inflammation in the anterior chamber in his right eye. He experienced an ocular trauma while using a grass mower 7 days -prior. Oral cephalosporine and ofloxacin eye drops were prescribed in a private clinic after trauma. He felt severe ocular pain and deterioration of vision and accompanying aggravation of the inflammation as the result of having too much to drink the day before his visit. He had an unremarkable medical history and no underlying illness.
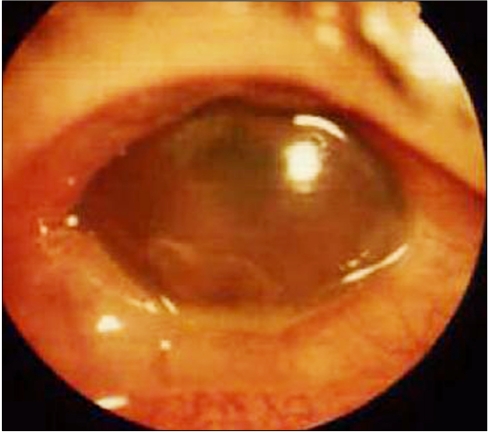
At the time of the initial visit, the patient's visual acuity was at the level of hand motion in the right eye and 1.0 in the left eye. The intraocular pressure (IOP) was 16 mmHg in the right eye and 10 mmHg in the left eye. The conjunctiva of the right eye was intensely injected with chemosis. Slit lamp examination showed corneal edema, 1 mm-length full thickness corneal laceration without leakage, 4+ cells and an inflamed membrane in the anterior chamber, 10% hypopyon, a mid-dilated-irregular pupil, posterior synechiae formation, and cataract change (Fig. 1). Fundus examination revealed a grade 4 vitreous opacity, and B-scan ultrasonography showed opacity in the anterior vitreous. An IOFB suspected as metallic material in the lens was identified upon orbital computerized tomography (Fig. 2). Initial laboratory analyses revealed a white blood cell count of 21,920 cells/mm3 (neutrophil, 89.9%).
We performed pars plana vitrectomy, phacoemulsification, foreign body removal, anterior chamber irrigation, suture of the corneal laceration, and intravitreal antibiotics injections of vancomycin (1 mg in 0.1 mL for Gram-positive coverage) and ceftazidime (2.25 mg in 0.1 mL for Gram-negative coverage). The foreign body in the lens was a piece of metal. During the operation, we aspirated some humor in the anterior chamber for identifying the causative bacterium and tests of antibiotic sensitivity.
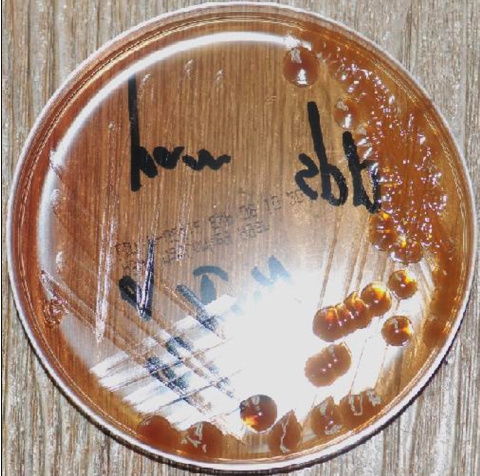
The day after operation, there were severe stromal edema and Descemet's membrand folds in the cornea and +3 to +4 cells, no hypopyon in the anterior chamber, and grade 3 vitreous opacity. The patient was treated with ciprofloxacin 200 mg (2 times/day) and tobramycin 80 mg (2 times/day) intravenously and fortified vancomycin (25 mg/mL), as well as moxifloxacin and tobramycin eye drops every 15 minutes. Three days postoperatively, no one was detected in Gram's staining, but Pantoea species grew in the culture of humor from the anterior chamber (Fig. 3). Using the VITEK 2 System (BioMerieux, Marcy l'Etoile, France) for antimicrobial susceptibility determination, the culture demonstrated susceptibility to ampicillin, aztreonam, cefotaxime, ceftazidime, ciprofloxacin, gentamicin, imipenem, peperacillin, and tobramycin, whereas resistance to ampicillin. Because the culture tested sensitive to antibiotics, the patient was given ceftazidime 1 g (2 times/day) intravenously, as well as fortified ceftazidime (50 mg/mL) and moxifloxacin eye drops every 15 minutes and oral prednisolone 45 mg daily with discontinuing vancomycin. Six days after operation, vitreous opacity and the red reflex degree worsened, so a repeat intravitreal antibiotics injection of ceftazidime (2 mg in 0.1 mL), as above, was performed.
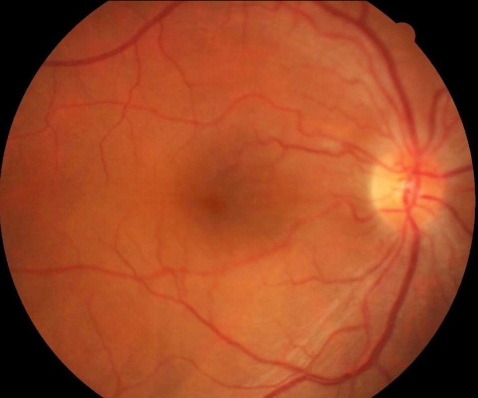
One week after last injection, the patient was noted to have +3 cells in the anterior chamber, grade +1 to +2 vitreous opacity, and IOP of 18 mmHg. Attempts at tapering oral corticosteroid and increasing the interval of eye drops progressed favorably without increasing inflammation. Two months after trauma, the best corrected visual acuity was 0.6, and no cells in the anterior chamber or vitreous opacity were detected (Fig. 4). He subsequently underwent a secondary IOL placement 4 months after trauma.
Post-traumatic endophthalmitis with retained IOFBs should attract great attention because of its high incidence and poor prognosis. Neuroimaging, preferably with non-contrast computed tomography, provides excellent information about IOFB size, shape, and location. Vitrectomy, which may reduce the incidence and the severity of endophthalmitis is suggested for the treatment of IOFBs and its complications and should be performed as soon as possible. Routine intravenous administration of antibiotics, combined with periocular injection and postoperative topical antibiotics, are recommended. Intravitreal antibiotics warrant consideration in patients with a positive Gram stain in cases of suspected endophthalmitis. A recent study reveals that the only benefit of adding intravitreal antibiotics was in eyes with IOFBs and in high-risk settings [1,2,9,10]. There was no significant difference in outcomes between Gram-positive, Gram-negative, and fungal infections in infectious endophthalmitis [11].
Bacteria of the family Enterobacteriaceae are important pathogens, causing intestinal and systemic illness of humans and other animals. Pantoea is a genus of Gram-negative aerobic bacteria of the family Enterobactoericeae, compromised of seven species and two subspecies. Within the genus, P. agglomerans is the most commonly isolated species in humans among not primary pathogens, but rather secondary opportunistic pathogens particularly in immunocompromised individuals. P. agglomerans is most associated with penetrating trauma by vegetative material, catheter-related bacteremia, and occupational exposure to airborne biological agents via the respiratory route when working with plants. P. agglomerans bacteremia has also been described in association with the contamination of intravenous fluid, total parenteral nutrition, the anesthetic agent propofol, and blood projects. There are reports of P. agglomerans infection, including arthritis or synovitis, osteromyelitis, ostitis, cholelithiasis, occupational respiratory infection, skin allergy, and peritonitis. In children, Pantoea species has a predilection for the lungs and infections may induce life-threatening conditions, such as septic shock and respiratory failure [12-16].
Pantoea ananatis causes disease symptoms in a wide range of economically important agricultural crops and forest tree species worldwide and could induce blood stream infection in elderly-human [13,17]. Pantoea has become known to be susceptible to tetracycline, as well as broad-spectrum cephalosporins, aminoglycosides, semisynthetic penicillins, and quinolones in most cases [16].
To date, there have been two reported cases of endophthalmitis caused by P. agglomerans [18,19]. One case involved an ensuing perforated cornea and endophthalmitis caused by injury to the left eye while gardening [18]. The lens was opaque, and its anterior capsule was ruptured. A culture of fluid obtained by anterior chamber paracentesis yielded a species of the Erwinia herbicolalathyri group (Enterobacter agglomerans). After extracapsular cataract extraction was performed and a course of cefazolin administered, the patient showed improvement. Another case reported involved metastatic endophthalmitis caused by the Gram-negative organism Enterobacter agglomerans following internal hemorrhoidal ligation [19]. The patient developed anterior uveitis that progressed to panophthalmitis, with a lenticular abscess and a necrotic retina. Despite aggressive surgery and appropriate antibiotic therapy, the affected eye lost useful vision.
A previously healthy 50-year-old man presented with endophthalmitis after ocular trauma. In response, vitrectomy, phacoemulsification, foreign body removal, anterior chamber irrigation, and intravitreal antibiotics injections of vancomycin and ceftazidime were performed. Pantoea species grew in a culture of humor from the anterior chamber. Antibiotic susceptibility revealed that there was no difference from established antibiotics sensitivity for Pantoea species. After proper antibiotics management, we achieved a favorable outcome.
REFERENCES
1. Jiang CH, Zhang MN. Traumatic endophthalmitis following penetrating ocular injuries with retained intraocular foreign bodies. Chin J Traumatol 2003;6:167-170.

2. Mieler WF, Ellis MK, Williams DF, Han DP. Retained intraocular foreign bodies and endophthalmitis. Ophthalmology 1990;97:1532-1538.


3. Thompson JT, Parver LM, Enger CL, et al. Infectious endophthalmitis after penetrating injuries with retained intraocular foreign bodies. National Eye Trauma System. Ophthalmology 1993;100:1468-1474.


4. Imrie FR, Cox A, Foot B, Macewen CJ. Surveillance of intraocular foreign bodies in the UK. Eye (Lond) 2008;22:1141-1147.


5. Cebulla CM, Flynn HW Jr. Endophthalmitis after open globe injuries. Am J Ophthalmol 2009;147:567-568.


6. Cruz AT, Cazacu AC, Allen CH. Pantoea agglomerans, a plant pathogen causing human disease. J Clin Microbiol 2007;45:1989-1992.



7. Deletoile A, Decre D, Courant S, et al. Phylogeny and identification of Pantoea species and typing of Pantoea agglomerans strains by multilocus gene sequencing. J Clin Microbiol 2009;47:300-310.


8. Brady C, Cleenwerck I, Venter S, et al. Phylogeny and identification of Pantoea species associated with plants, humans and the natural environment based on multilocus sequence analysis (MLSA). Syst Appl Microbiol 2008;31:447-460.


9. Yeh S, Colyer MH, Weichel ED. Current trends in the management of intraocular foreign bodies. Curr Opin Ophthalmol 2008;19:225-233.


10. Andreoli CM, Andreoli MT, Kloek CE, et al. Low rate of endophthalmitis in a large series of open globe injuries. Am J Ophthalmol 2009;147:601-608.e2.


11. Fan JC, Niederer RL, von Lany H, Polkinghorne PJ. Infectious endophthalmitis: clinical features, management and visual outcomes. Clin Experiment Ophthalmol 2008;36:631-636.


12. Chale-Matsau JR, Snyman HG. The survival of pathogens in soil treated with wastewater sludge and in potatoes grown in such soil. Water Sci Technol 2006;54:163-168.

13. Van Rostenberghe H, Noraida R, Wan Pauzi WI, et al. The clinical picture of neonatal infection with Pantoea species. Jpn J Infect Dis 2006;59:120-121.


14. Gora A, Mackiewicz B, Krawczyk P, et al. Occupational exposure to organic dust, microorganisms, endotoxin and peptidoglycan among plants processing workers in Poland. Ann Agric Environ Med 2009;16:143-150.

15. Sanders WE Jr, Sanders CC. Enterobacter spp.: pathogens poised to flourish at the turn of the century. Clin Microbiol Rev 1997;10:220-241.



16. Kim HO, Lee HJ, Kim DW, et al. A case of peritonitis caused by Pantoea agglomerans in a patient undergoing continuous ambulatory peritoneal dialysis. Korean J Med 2008;74:426-429.
17. Coutinho TA, Venter SN. Pantoea ananatis: an unconventional plant pathogen. Mol Plant Pathol 2009;10:325-335.







 PDF Links
PDF Links PubReader
PubReader Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print




